Final ID: Mo3078
Geographical Disparities in Peripartum Cardiomyopathy: A Nationwide Study
Abstract Body (Do not enter title and authors here): Background: Previous studies have reported disparities in maternal cardiovascular health across different U.S. regions; however, the impact of geographic variation on outcomes in peripartum cardiomyopathy (PPCM) remains poorly understood.
Objective: To evaluate geographic variations in outcomes of PPCM across U.S. census regions, focusing on sociodemographic and clinical risk factors.
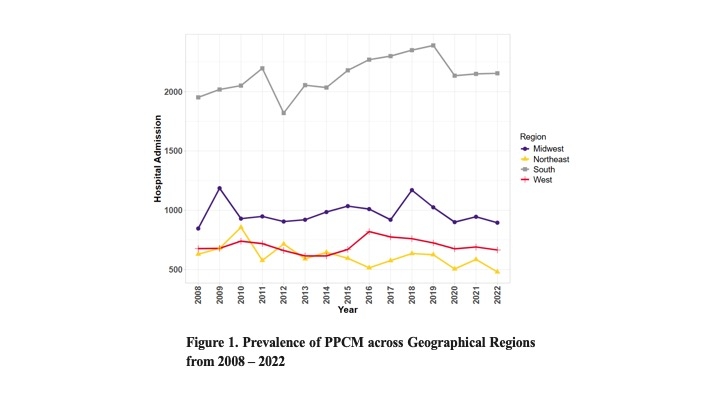
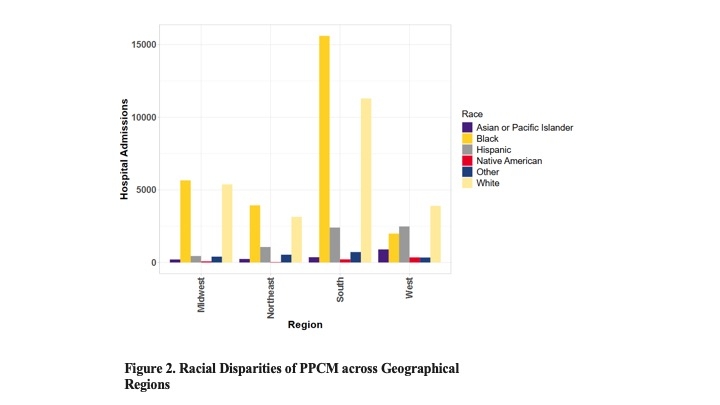
Methods: This retrospective study analyzed 2008–2022 data from the National Inpatient Sample (NIS), encompassing 66,368 weighted PPCM hospitalizations. Baseline characteristics across geographical regions were analyzed using descriptive statistics and chi-square tests. Multivariable logistic regression evaluated associations between geographical regions and in-hospital mortality outcomes, adjusting for race, income, and comorbidities.
Results: Among 66,368 weighted PPCM hospitalizations, the South accounted for 48.3% of PPCM cases, followed by the Midwest (22.0%), West (15.8%), and Northeast (13.9%; p<0.001). Black patients comprised 51% of Southern cases vs. 37% in non-Southern regions (p<0.001). Southern cases were disproportionately from the lowest income quartile (47% vs 36%; p<0.001). Southern populations demonstrated statistically significant comorbidity burdens, including hypertension (45.9% vs 37.7%, p<0.001), obesity (26.0% vs 23.6%, p<0.001), and chronic kidney disease (6.1% vs 5.2%, p=0.02). Geographical analysis of PPCM mortality revealed significant disparities, with Southern residence associated with 40% higher adjusted odds of mortality compared to other regions (aOR=1.40, 95% CI=1.04–1.87, p=0.025) after controlling for race, income, and comorbidities. Black race (aOR=1.83, 95% CI=1.26–2.65, p=0.001) and chronic kidney disease (aOR=3.81, 95% CI=2.53–5.73, p<0.001) were key predictors. Interestingly, hypertension was associated with lower odds of mortality (aOR=0.53, 95% CI= 0.37–0.75, p<0.001).
Conclusion: Geographical disparities in in-hospital mortality of PPCM persist after adjustment for socioeconomic and clinical factors, with the Southern U.S. demonstrating a significantly elevated burden. Addressing systemic drivers of regional inequities is critical to improving maternal cardiovascular outcomes.
Objective: To evaluate geographic variations in outcomes of PPCM across U.S. census regions, focusing on sociodemographic and clinical risk factors.
Methods: This retrospective study analyzed 2008–2022 data from the National Inpatient Sample (NIS), encompassing 66,368 weighted PPCM hospitalizations. Baseline characteristics across geographical regions were analyzed using descriptive statistics and chi-square tests. Multivariable logistic regression evaluated associations between geographical regions and in-hospital mortality outcomes, adjusting for race, income, and comorbidities.
Results: Among 66,368 weighted PPCM hospitalizations, the South accounted for 48.3% of PPCM cases, followed by the Midwest (22.0%), West (15.8%), and Northeast (13.9%; p<0.001). Black patients comprised 51% of Southern cases vs. 37% in non-Southern regions (p<0.001). Southern cases were disproportionately from the lowest income quartile (47% vs 36%; p<0.001). Southern populations demonstrated statistically significant comorbidity burdens, including hypertension (45.9% vs 37.7%, p<0.001), obesity (26.0% vs 23.6%, p<0.001), and chronic kidney disease (6.1% vs 5.2%, p=0.02). Geographical analysis of PPCM mortality revealed significant disparities, with Southern residence associated with 40% higher adjusted odds of mortality compared to other regions (aOR=1.40, 95% CI=1.04–1.87, p=0.025) after controlling for race, income, and comorbidities. Black race (aOR=1.83, 95% CI=1.26–2.65, p=0.001) and chronic kidney disease (aOR=3.81, 95% CI=2.53–5.73, p<0.001) were key predictors. Interestingly, hypertension was associated with lower odds of mortality (aOR=0.53, 95% CI= 0.37–0.75, p<0.001).
Conclusion: Geographical disparities in in-hospital mortality of PPCM persist after adjustment for socioeconomic and clinical factors, with the Southern U.S. demonstrating a significantly elevated burden. Addressing systemic drivers of regional inequities is critical to improving maternal cardiovascular outcomes.
More abstracts on this topic:
Comparison of Long-Term Outcomes With Metoprolol vs Carvedilol in Women With Peripartum Cardiomyopathy: A Propensity-Matched Analysis
Yeo Yong Hao, Vignarajah Aravinthan, Wong Hermon Kha Kin, Ong Tze Ern, Tamirisa Kamala, Davis Melinda
Feto-maternal outcomes of subsequent pregnancy among women with Peripartum Cardiomyopathy in Tanzania.Pallangyo Pedro, Mkojera Zabella, Komba Makrina, Kisenge Peter Richard