Final ID: Mo3132
Endovascular Treatment Versus Best Medical Therapy for Acute Ischemic Stroke Due to Medium or Distal Vessel Occlusions: A Meta-Analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background:
The role of endovascular treatment (EVT) in acute ischemic stroke due to medium or distal vessel occlusions remains uncertain, with limited randomized evidence guiding clinical decision-making. This meta-analysis evaluates the efficacy and safety of EVT compared to best medical therapy (BMT) in this patient population.
Methods:
We systematically searched PubMed, Embase, and Cochrane Library for randomized controlled trials comparing EVT with BMT for acute ischemic stroke due to medium or distal vessel occlusions. Primary outcomes included all-cause mortality and favorable functional outcome defined by modified Rankin Scale (mRS) scores. Secondary outcomes included excellent functional outcome (mRS 0–1 at 90 days) and symptomatic intracranial hemorrhage (sICH). Pooled risk ratios (RRs) and 95% confidence intervals (CIs) were calculated using a random-effects model.
Results:
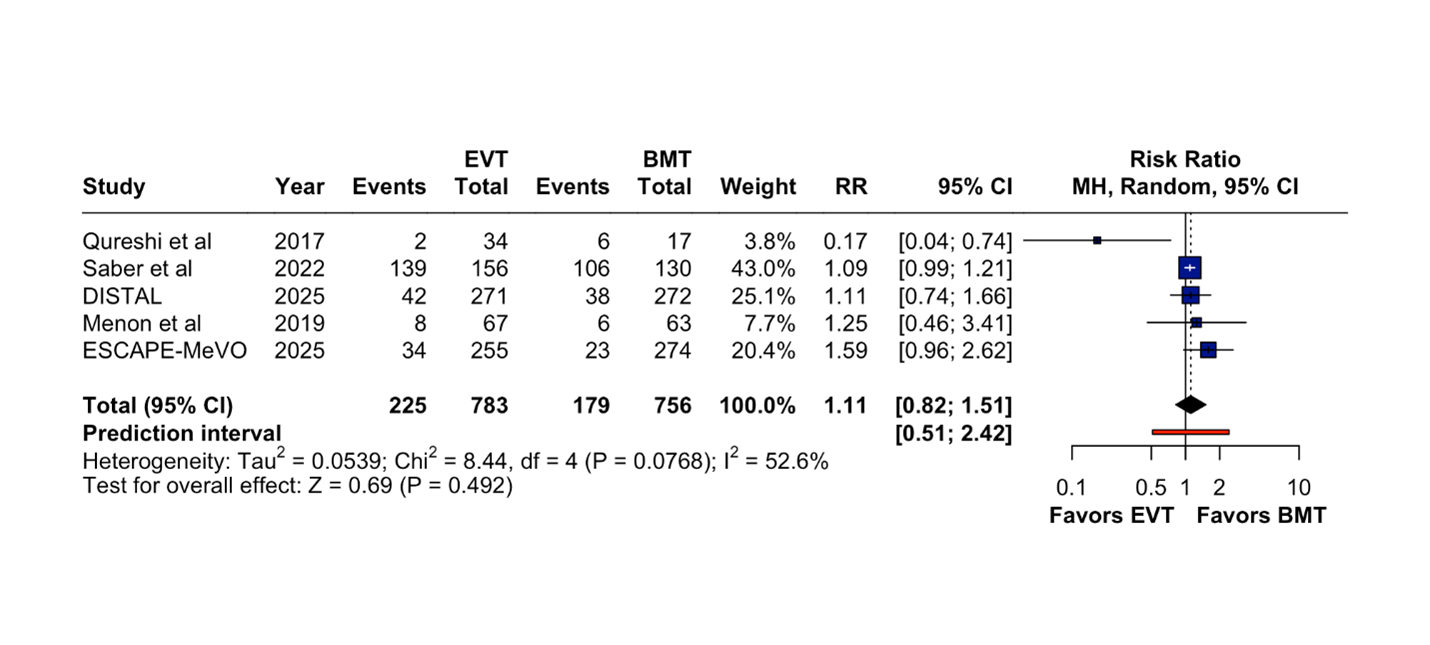
Five randomized controlled trials were included with 1,539 patients (783 EVT, 756 BMT). The mean age of the included studies was 73.4 years, while 56.6 % of the included studies were males. EVT was not associated with a significant reduction in all-cause mortality compared to BMT (RR = 1.11; 95% CI: 0.82–1.51; P = 0.492; I2 = 52.6%; Figure 1). Excellent functional outcome (mRS 0–1) was similar between groups (RR = 1.02; 95% CI: 0.90–1.16; P = 0.716; I2 = 39.6%). Likewise, favorable functional outcome (mRS 0–2) did not significantly differ (RR = 1.03; 95% CI: 0.90–1.18; P = 0.645; I2 = 50.0%). There was no significant difference in the incidence of sICH (RR = 1.30; 95% CI: 0.13–12.89; P = 0.822), although this analysis showed considerable heterogeneity (I2 = 96.1%).
Conclusion:
In patients with stroke due to medium or distal vessel occlusions, EVT did not significantly improve mortality or functional outcomes compared to BMT. The risk of sICH was not significantly increased, though safety data were limited by heterogeneity. Further large-scale trials are needed to clarify the clinical benefits of EVT in this subgroup.
The role of endovascular treatment (EVT) in acute ischemic stroke due to medium or distal vessel occlusions remains uncertain, with limited randomized evidence guiding clinical decision-making. This meta-analysis evaluates the efficacy and safety of EVT compared to best medical therapy (BMT) in this patient population.
Methods:
We systematically searched PubMed, Embase, and Cochrane Library for randomized controlled trials comparing EVT with BMT for acute ischemic stroke due to medium or distal vessel occlusions. Primary outcomes included all-cause mortality and favorable functional outcome defined by modified Rankin Scale (mRS) scores. Secondary outcomes included excellent functional outcome (mRS 0–1 at 90 days) and symptomatic intracranial hemorrhage (sICH). Pooled risk ratios (RRs) and 95% confidence intervals (CIs) were calculated using a random-effects model.
Results:
Five randomized controlled trials were included with 1,539 patients (783 EVT, 756 BMT). The mean age of the included studies was 73.4 years, while 56.6 % of the included studies were males. EVT was not associated with a significant reduction in all-cause mortality compared to BMT (RR = 1.11; 95% CI: 0.82–1.51; P = 0.492; I2 = 52.6%; Figure 1). Excellent functional outcome (mRS 0–1) was similar between groups (RR = 1.02; 95% CI: 0.90–1.16; P = 0.716; I2 = 39.6%). Likewise, favorable functional outcome (mRS 0–2) did not significantly differ (RR = 1.03; 95% CI: 0.90–1.18; P = 0.645; I2 = 50.0%). There was no significant difference in the incidence of sICH (RR = 1.30; 95% CI: 0.13–12.89; P = 0.822), although this analysis showed considerable heterogeneity (I2 = 96.1%).
Conclusion:
In patients with stroke due to medium or distal vessel occlusions, EVT did not significantly improve mortality or functional outcomes compared to BMT. The risk of sICH was not significantly increased, though safety data were limited by heterogeneity. Further large-scale trials are needed to clarify the clinical benefits of EVT in this subgroup.
More abstracts on this topic:
Association of pre-thrombectomy infarct topography and hemorrhagic transformation in patients with acute ischemic stroke: A multicenter Bayesian analysis
Bonkhoff Anna, Simonsen Claus, Patel Aman, Rost Natalia, Regenhardt Robert, Schirmer Markus, Favilla Christopher, Das Alvin, Dmytriw Adam, Gupta Rajiv, Rabinov James, Stapleton Christopher, Leslie-mazwi Thabele
Higher t-PA Doses are Associated with Reduced In-Hospital Mortality in Pulmonary Embolism Patients Undergoing Catheter-Directed ThrombolysisHinkamp Colin, Liu Jason, Nardi Matthew, Postalian Alexander, Nair Ajith, Segar Matthew