Final ID: Mo1017
Nonlinear Association Between Post-Cardiac Arrest Mean Arterial Pressure and Outcome Suggests 85–100 mmHg as the Optimal Range
Abstract Body (Do not enter title and authors here): Introduction
Post-cardiac arrest care seeks to optimize cerebral perfusion for neurological recovery. Mean arterial pressure (MAP) is a key target in hemodynamic management, but guidelines recommend only a minimal threshold of 60–65 mmHg based on low-certainty evidence. Observational studies report better outcomes with higher MAP, but cannot prove causality. In contrast, randomized controlled trials (RCTs) that adjust MAP show inconsistent results. This discrepancy may reflect confounding in observational data, where higher MAP often indicates lower illness severity, and harm from excessive MAP in some RCT patients. Both study types dichotomized MAP, assuming a linear relationship. However, because both hypotension and hypertension may worsen outcomes, a nonlinear association is plausible. Identifying an optimal MAP range instead of using cutoffs may improve outcomes.
Aims
We aimed to identify an optimal MAP range associated with the highest probability of neurological recovery, assuming a nonlinear relationship between MAP and outcome.
Methods
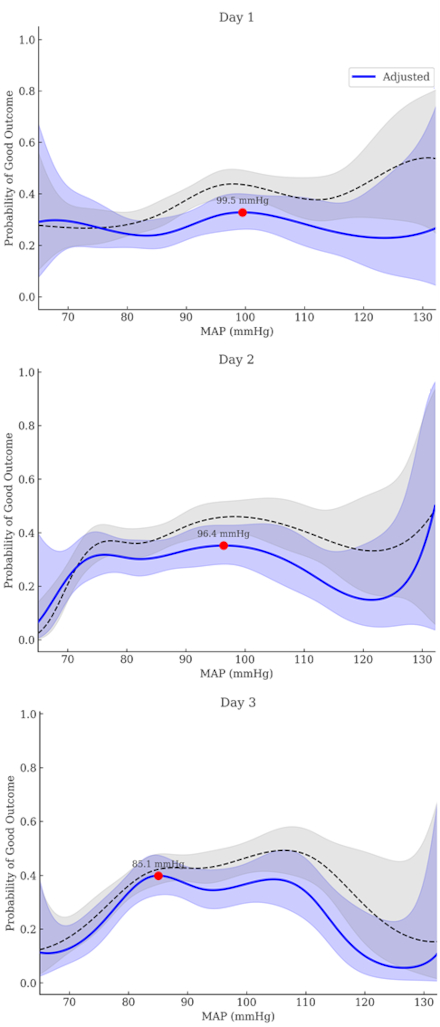
We analyzed data from 1,146 out-of-hospital cardiac arrest survivors in the Korean Hypothermia Network prospective registry. MAPs were calculated for Day 1 (0–24h), Day 2 (30–48h), Day 3 (54–72h), and after return of spontaneous circulation. Restricted cubic spline (RCS) logistic regression modeled nonlinear associations between MAP and good neurological outcome (modified Rankin Scale 0–2 at 6 months). Optimal MAP ranges were derived from spline curves. Logistic regression evaluated associations between maintaining MAP within this range and outcomes, including 6-month survival.
Results
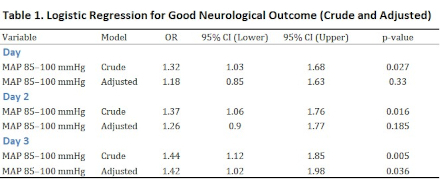
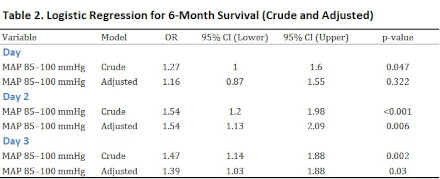
RCS analysis showed a nonlinear association between MAP and neurological outcome across all time intervals. The MAP values associated with the highest predicted probability of good outcome were 99.5 mmHg on Day 1, 96.4 mmHg on Day 2, and 85.1 mmHg on Day 3. Based on these, the optimal MAP range was defined as 85–100 mmHg. Maintaining MAP within this range was significantly associated with good neurological outcome on Day 3 (adjusted OR 1.42, p = 0.036) and improved survival on Day 2 (adjusted OR 1.54, p = 0.006) and Day 3 (adjusted OR 1.39, p = 0.030).
Conclusion
MAP and neurological outcome after cardiac arrest appear nonlinearly related. Maintaining MAP between 85 and 100 mmHg was associated with improved neurological recovery and survival, particularly on Days 2 and 3. This range warrants further investigation in interventional trials.
Post-cardiac arrest care seeks to optimize cerebral perfusion for neurological recovery. Mean arterial pressure (MAP) is a key target in hemodynamic management, but guidelines recommend only a minimal threshold of 60–65 mmHg based on low-certainty evidence. Observational studies report better outcomes with higher MAP, but cannot prove causality. In contrast, randomized controlled trials (RCTs) that adjust MAP show inconsistent results. This discrepancy may reflect confounding in observational data, where higher MAP often indicates lower illness severity, and harm from excessive MAP in some RCT patients. Both study types dichotomized MAP, assuming a linear relationship. However, because both hypotension and hypertension may worsen outcomes, a nonlinear association is plausible. Identifying an optimal MAP range instead of using cutoffs may improve outcomes.
Aims
We aimed to identify an optimal MAP range associated with the highest probability of neurological recovery, assuming a nonlinear relationship between MAP and outcome.
Methods
We analyzed data from 1,146 out-of-hospital cardiac arrest survivors in the Korean Hypothermia Network prospective registry. MAPs were calculated for Day 1 (0–24h), Day 2 (30–48h), Day 3 (54–72h), and after return of spontaneous circulation. Restricted cubic spline (RCS) logistic regression modeled nonlinear associations between MAP and good neurological outcome (modified Rankin Scale 0–2 at 6 months). Optimal MAP ranges were derived from spline curves. Logistic regression evaluated associations between maintaining MAP within this range and outcomes, including 6-month survival.
Results
RCS analysis showed a nonlinear association between MAP and neurological outcome across all time intervals. The MAP values associated with the highest predicted probability of good outcome were 99.5 mmHg on Day 1, 96.4 mmHg on Day 2, and 85.1 mmHg on Day 3. Based on these, the optimal MAP range was defined as 85–100 mmHg. Maintaining MAP within this range was significantly associated with good neurological outcome on Day 3 (adjusted OR 1.42, p = 0.036) and improved survival on Day 2 (adjusted OR 1.54, p = 0.006) and Day 3 (adjusted OR 1.39, p = 0.030).
Conclusion
MAP and neurological outcome after cardiac arrest appear nonlinearly related. Maintaining MAP between 85 and 100 mmHg was associated with improved neurological recovery and survival, particularly on Days 2 and 3. This range warrants further investigation in interventional trials.
More abstracts on this topic:
A pilot study of an intervention for self-management of blood pressure among refugees fleeing war and resettled in the United States
Behnam Rawnaq, Godino Job, Celis Deisy, Anderson Cheryl, Al-rousan Tala
Association of Pittsburgh Cardiac Arrest Category with death due to withdrawal of life-sustaining therapyTam Jonathan, Callaway Clifton