Final ID: Su3031
Impact of Early Reimplantation after Transvenous Lead Extraction of Infected Cardiac Implantable Electronic Device
Abstract Body (Do not enter title and authors here): ABSTRACT
Background
Transvenous lead extraction (TLE) is the standard of care for cardiac implantable electronic device (CIED) infections. Data regarding the optimal timing of CIED reimplantation after TLE are not well established.
Objective
This study aims to assess the 5-year outcomes of early (≤7 days) versus non-early (>7 days) CIED reimplantation following TLE for CIED infection using a multi-national database.
Methods
Using the TriNetX Analytics Research Network, we included patients aged ≥18 years who underwent TLE for CIED infection between 1/1/2014 and 1/1/2020. Patients were further categorized into two groups: early CIED reimplantation (≤7 days from TLE) and non-early CIED reimplantation. Propensity score matching (PSM) was performed by including patient demographics, LVEF, cardiac comorbidities and medications. The study outcomes included all-cause mortality and cardiac adverse events during a 5-year study period.
Results
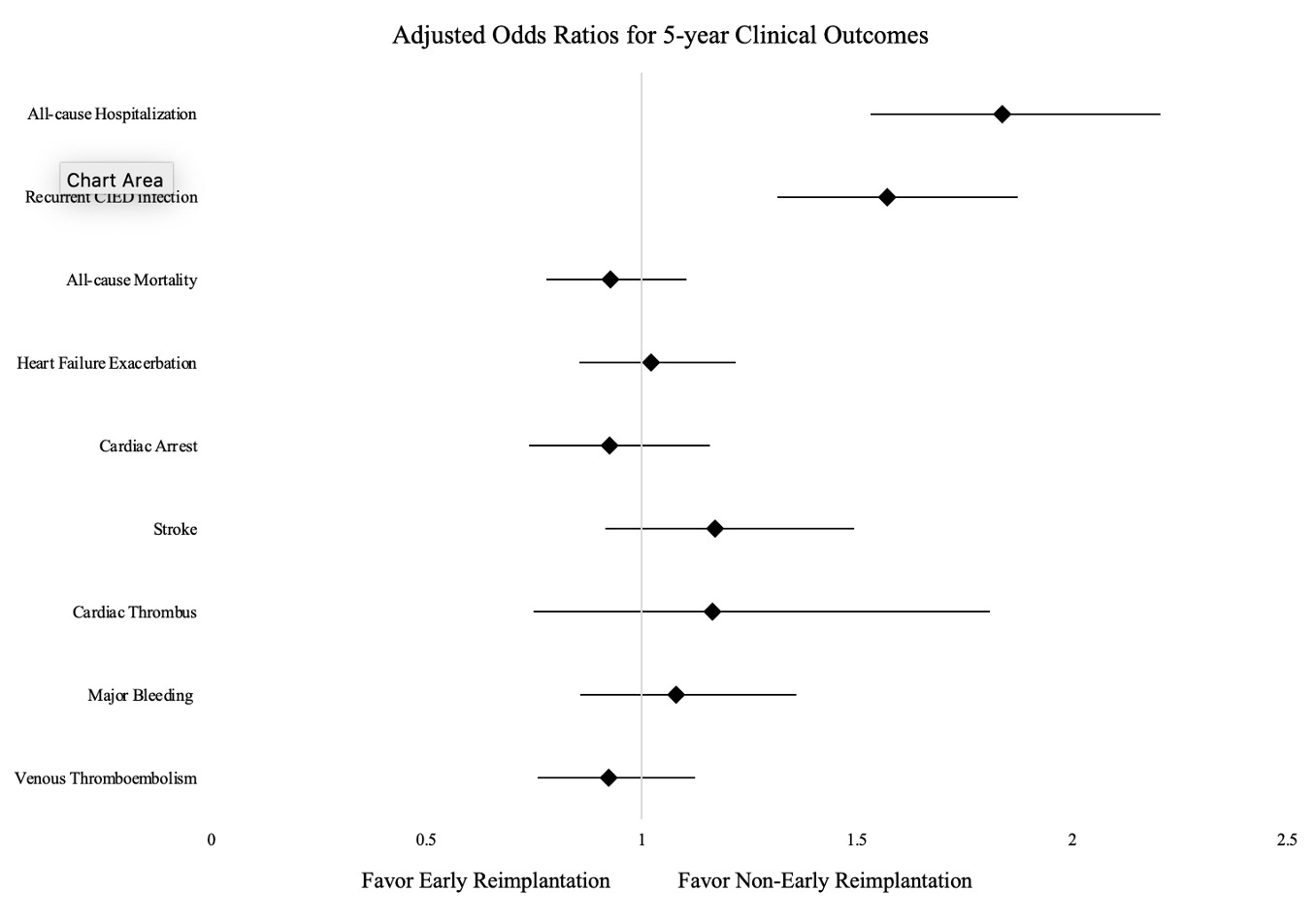
A total of 1668 patients in the early CIED reimplantation group and 1550 in the non-early group were identified. After PSM, 1327 patients in each group were analyzed. Compared to non-early group, early CIED reimplantation group was associated with significantly higher odds of all-cause hospitalization (odds ratio [OR]: 1.837, 95% confidence interval [CI]: 1.532-2.203) and repeated device infection (OR: 1.569, 95% CI: 1.314-1.873) at 5-year follow-up. However, no significant differences were observed in all-cause mortality (OR: 0.927, 95% CI: 0.778-1.104), HF exacerbation (OR: 1.021, 95% CI: 0.855-1.218), cardiac arrest (OR:0.924, 95% CI: 0.739-1.157), stroke (OR: 1.169, 95% CI: 0.915-1.494), cardiac thrombus (OR: 1.163, 95% CI: 0.749-1.808), major bleeding (OR: 1.079, 95% CI: 0.857-1.358) and venous thromboembolism (OR: 0.923, 95% CI: 0.759-1.123) between the two groups.
Conclusion
Early reimplantation of CIED following TLE of infected devices was associated with worse outcomes in all-cause hospitalization and repeated device infection. Further large prospective studies are needed to define the optimal timing of device reimplantation.
Background
Transvenous lead extraction (TLE) is the standard of care for cardiac implantable electronic device (CIED) infections. Data regarding the optimal timing of CIED reimplantation after TLE are not well established.
Objective
This study aims to assess the 5-year outcomes of early (≤7 days) versus non-early (>7 days) CIED reimplantation following TLE for CIED infection using a multi-national database.
Methods
Using the TriNetX Analytics Research Network, we included patients aged ≥18 years who underwent TLE for CIED infection between 1/1/2014 and 1/1/2020. Patients were further categorized into two groups: early CIED reimplantation (≤7 days from TLE) and non-early CIED reimplantation. Propensity score matching (PSM) was performed by including patient demographics, LVEF, cardiac comorbidities and medications. The study outcomes included all-cause mortality and cardiac adverse events during a 5-year study period.
Results
A total of 1668 patients in the early CIED reimplantation group and 1550 in the non-early group were identified. After PSM, 1327 patients in each group were analyzed. Compared to non-early group, early CIED reimplantation group was associated with significantly higher odds of all-cause hospitalization (odds ratio [OR]: 1.837, 95% confidence interval [CI]: 1.532-2.203) and repeated device infection (OR: 1.569, 95% CI: 1.314-1.873) at 5-year follow-up. However, no significant differences were observed in all-cause mortality (OR: 0.927, 95% CI: 0.778-1.104), HF exacerbation (OR: 1.021, 95% CI: 0.855-1.218), cardiac arrest (OR:0.924, 95% CI: 0.739-1.157), stroke (OR: 1.169, 95% CI: 0.915-1.494), cardiac thrombus (OR: 1.163, 95% CI: 0.749-1.808), major bleeding (OR: 1.079, 95% CI: 0.857-1.358) and venous thromboembolism (OR: 0.923, 95% CI: 0.759-1.123) between the two groups.
Conclusion
Early reimplantation of CIED following TLE of infected devices was associated with worse outcomes in all-cause hospitalization and repeated device infection. Further large prospective studies are needed to define the optimal timing of device reimplantation.
More abstracts on this topic:
4D Cardiac Optogenetics Enable Complex Arrhythmia Modelling and Precise Interventional Simulation
Wexler Yehuda, Grinstein Harel, Landesberg Michal, Glatstein Shany, Huber Irit, Arbel Gil, Gepstein Lior
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart FailureO'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja