Final ID: MP2140
Prevalence of Masked Hypertension Assessed by Home Blood Pressure Monitoring According to AHA PREVENT Risk Estimation Among Japanese Outpatients
Abstract Body (Do not enter title and authors here): BACKGROUND: Masked hypertension (MHT) is defined as high out-of-office blood pressure (BP) despite non-high office BP and is associated with incident cardiovascular disease (CVD). The 2017 ACC/AHA hypertension guideline recommends assessing CVD risk using the 2013 Pooled Cohort Equations (PCE). In 2023, the AHA released a newer model, the Predicting Risk of CVD EVENTs (PREVENT). If these prediction models can help identify MHT, they may improve patient selection for out-of-office BP assessment.
HYPOTHESIS: A higher estimated CVD risk according to PREVENT or PCE is associated with a higher prevalence of MHT than a lower estimated risk.
METHODS: This cross-sectional analysis used data from a nationwide cohort designed to evaluate home BP for CVD prediction among 4,310 Japanese outpatients. Home BP was measured with a validated oscillometric device twice daily (morning and evening) for 14 days. MHT was defined as high home BP (systolic BP [SBP] ≥135 mmHg and/or diastolic BP [DBP] ≥85 mmHg) despite non-high clinic BP (SBP <140 mmHg and DBP <90 mmHg). Participants with prior atherosclerotic CVD (ASCVD), heart failure, or ineligibility for the PREVENT and PCE models were excluded. Estimated risks were calculated using the PREVENT 10-year total CVD (PREVENTtotal CVD) and ASCVD (PREVENTASCVD) models and the PCE 10-year ASCVD (PCEASCVD) model.
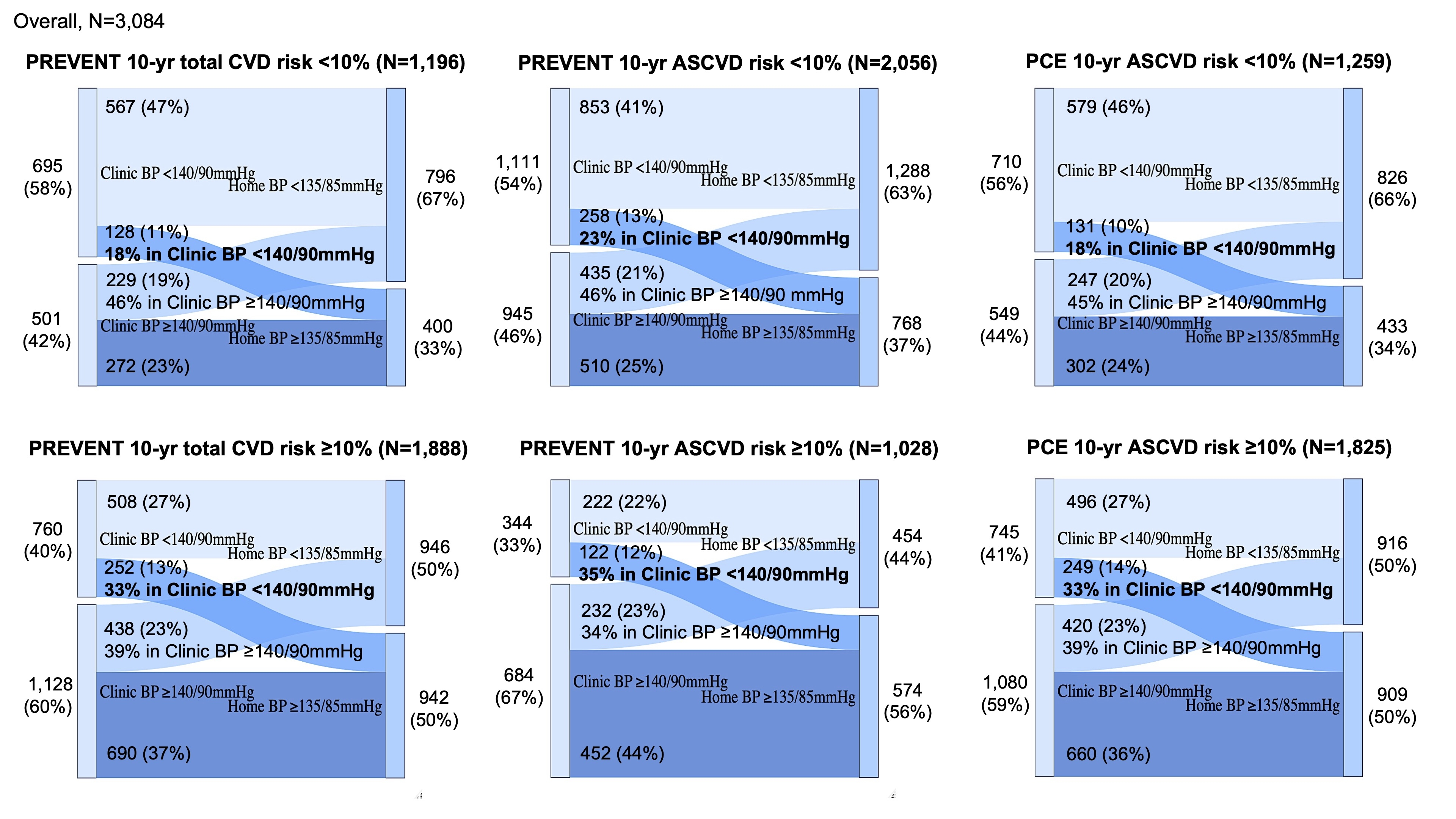
RESULTS: Among 3,084 participants (mean age, 63.5 years; 44% male; 77% use antihypertensive medication), 61%, 33%, and 59% had an estimated risk ≥10% according to the PREVENTtotalCVD, PREVENTASCVD, and PCEASCVD, respectively. Figure shows clinic and home BP status stratified by an estimated risk of <10% or ≥10% according to each model. Of 1,445 participants with non-high clinic BP, the prevalence of MHT was 33% versus 18% in those with an estimated risk ≥10% versus <10% by PREVENTtotal CVD. In adjusted logistic models, the odds ratios (ORs) for MHT in participants with ≥10% by PREVENTtotalCVD (OR 1.71, 95%CI 1.17-2.49), by PREVENTASCVD (OR 1.05, 95%CI 0.73-1.53), and by PCEASCVD (OR 2.09, 95%CI 1.42-3.09) compared with those with <10%. The C-statistics for discriminating MHT were not different between models including each estimated risk as a continuous variable (C-statistics: PREVENTtotal CVD, 0.661; PREVENTASCVD, 0.663; and PCEASCVD, 0.662).
CONCLUSIONS: In the present study, estimated CVD risk according to the both PREVENT and PCE models was associated with the prevalence of MHT.
HYPOTHESIS: A higher estimated CVD risk according to PREVENT or PCE is associated with a higher prevalence of MHT than a lower estimated risk.
METHODS: This cross-sectional analysis used data from a nationwide cohort designed to evaluate home BP for CVD prediction among 4,310 Japanese outpatients. Home BP was measured with a validated oscillometric device twice daily (morning and evening) for 14 days. MHT was defined as high home BP (systolic BP [SBP] ≥135 mmHg and/or diastolic BP [DBP] ≥85 mmHg) despite non-high clinic BP (SBP <140 mmHg and DBP <90 mmHg). Participants with prior atherosclerotic CVD (ASCVD), heart failure, or ineligibility for the PREVENT and PCE models were excluded. Estimated risks were calculated using the PREVENT 10-year total CVD (PREVENTtotal CVD) and ASCVD (PREVENTASCVD) models and the PCE 10-year ASCVD (PCEASCVD) model.
RESULTS: Among 3,084 participants (mean age, 63.5 years; 44% male; 77% use antihypertensive medication), 61%, 33%, and 59% had an estimated risk ≥10% according to the PREVENTtotalCVD, PREVENTASCVD, and PCEASCVD, respectively. Figure shows clinic and home BP status stratified by an estimated risk of <10% or ≥10% according to each model. Of 1,445 participants with non-high clinic BP, the prevalence of MHT was 33% versus 18% in those with an estimated risk ≥10% versus <10% by PREVENTtotal CVD. In adjusted logistic models, the odds ratios (ORs) for MHT in participants with ≥10% by PREVENTtotalCVD (OR 1.71, 95%CI 1.17-2.49), by PREVENTASCVD (OR 1.05, 95%CI 0.73-1.53), and by PCEASCVD (OR 2.09, 95%CI 1.42-3.09) compared with those with <10%. The C-statistics for discriminating MHT were not different between models including each estimated risk as a continuous variable (C-statistics: PREVENTtotal CVD, 0.661; PREVENTASCVD, 0.663; and PCEASCVD, 0.662).
CONCLUSIONS: In the present study, estimated CVD risk according to the both PREVENT and PCE models was associated with the prevalence of MHT.
More abstracts on this topic:
A Qualitative Study of Perspectives on South Asian Dietary Practices: Exploring a Framework for Culturally Tailored Food-is-Medicine Interventions
Kaloth Srivarsha, Fitzgerald Nurgul, Bacalia Karen Mae, Kalbag Aparna, Setoguchi Soko
Blood pressure and heart rate patterns of patients diagnosed with acute coronary syndrome and underwent percutaneous coronary interventionLeowattana Tawithep, Phoopattana Supamongkol, Sricholwattana Suchat, Krisnangkura Pakawat, Wongsoasu Arthit, Rattanajaruskul Nattapun, Rungsangmanoon Worawut, Angkananard Teeranan