Final ID: MP1210
Noninvasive Respiratory Support After Cardiothoracic Surgery: A Network Meta-analysis
Abstract Body (Do not enter title and authors here): Background
Cardiothoracic surgery is associated with a high incidence of postoperative respiratory complications arising from a combination of patient-related and procedural risk factors. Although noninvasive respiratory support strategies, including high-flow nasal cannula (HFNC), noninvasive positive pressure ventilation (NIPPV), and conventional oxygen therapy (COT), are commonly used to reduce post-extubation complications, their relative effectiveness in this population remains uncertain.
Methods
We conducted a comprehensive search of Embase, PubMed, and Scopus between January 2010 and December 2024 to identify randomized controlled trials that compared the efficacy of HFNC, COT and NIPPV in adult patients following CTS. A frequentist network meta-analysis was performed. Outcomes included reintubation rate, in-hospital mortality, ICU and hospital length of stay, pneumonia incidence, CPAP requirement, and PaCO2 levels.
Results
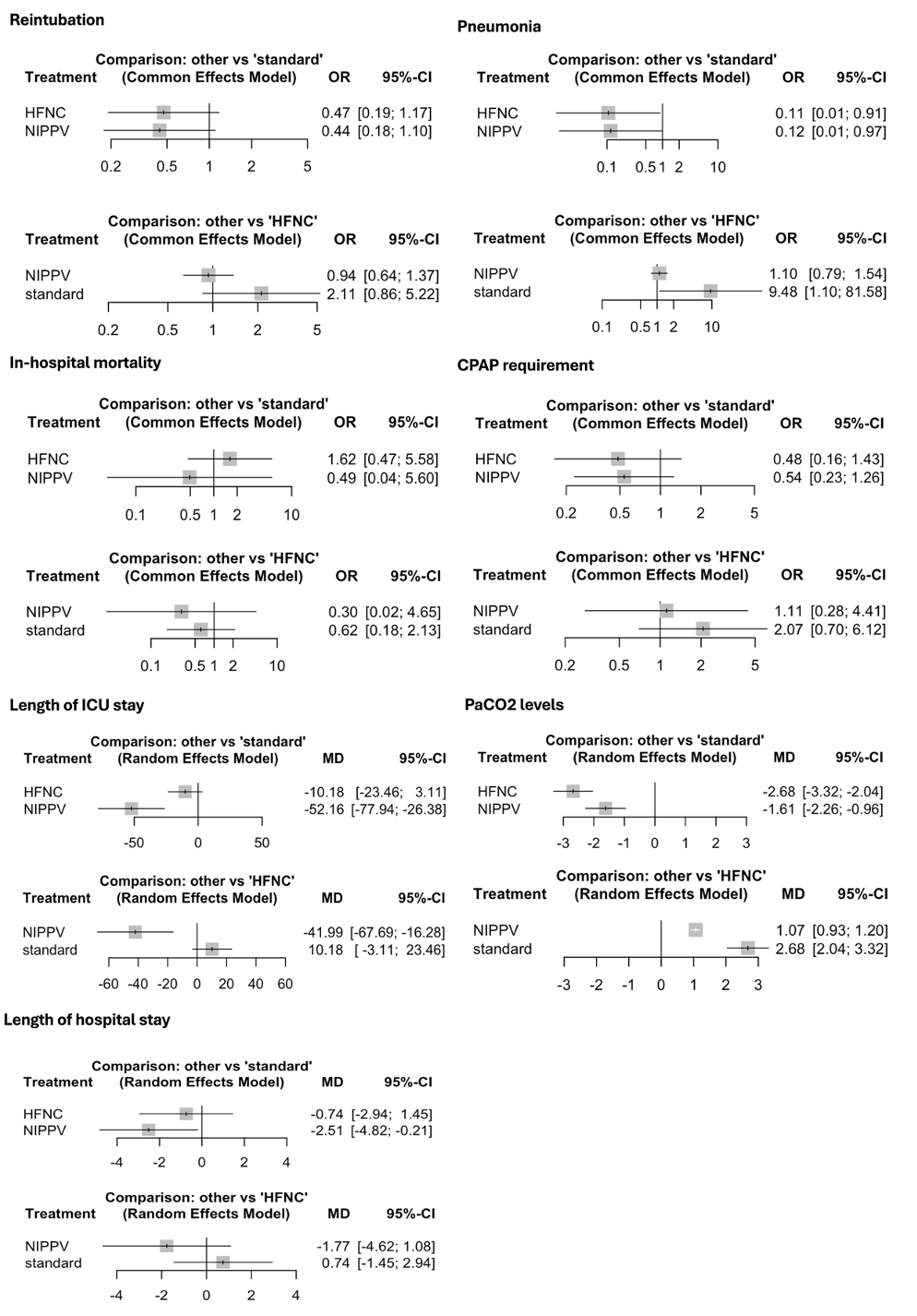
Eleven RCTs enrolling 1,664 patients were analyzed. There were no statistically significant differences in reintubation rates, in-hospital mortality, or CPAP requirements between HFNC and COT, NIPPV and COT, or NIPPV and HFNC. NIPPV significantly reduced ICU length of stay compared to both COT (MD –52.16 hours; 95% CI, –77.94 to –26.38) and HFNC (MD –41.99 hours; 95% CI, –67.69 to –16.28), and also shortened hospital length of stay compared to COT (MD –2.51 days; 95% CI, –4.82 to –0.21). Both HFNC and NIPPV were associated with a significantly lower incidence of pneumonia compared to COT (HFNC: OR 0.11; 95% CI, 0.01 to 0.91; NIPPV: OR 0.12; 95% CI, 0.01 to 0.97). In terms of PaCO2 reduction, both HFNC and NIPPV significantly lowered levels compared with COT (HFNC: MD –2.68 mmHg; 95% CI, –3.32 to –2.04; NIPPV: MD –1.61 mmHg; 95% CI, –2.26 to –0.96), with HFNC showing a greater reduction than NIPPV (MD 1.07 mmHg; 95% CI, 0.93 to 1.20).
Conclusion
In adult patients undergoing cardiothoracic surgery, the rates of reintubation and in-hospital mortality were similar across noninvasive respiratory support strategies. NIPPV may reduce ICU and hospital length of stay compared with HFNC and COT, while both HFNC and NIPPV may lower the incidence of pneumonia relative to COT. Although these findings support the use of HFNC or NIPPV over COT, the lack of significant differences in key clinical outcomes and overall low certainty of evidence underscores the need for further high-quality randomized trials to clarify their comparative effectiveness.
Cardiothoracic surgery is associated with a high incidence of postoperative respiratory complications arising from a combination of patient-related and procedural risk factors. Although noninvasive respiratory support strategies, including high-flow nasal cannula (HFNC), noninvasive positive pressure ventilation (NIPPV), and conventional oxygen therapy (COT), are commonly used to reduce post-extubation complications, their relative effectiveness in this population remains uncertain.
Methods
We conducted a comprehensive search of Embase, PubMed, and Scopus between January 2010 and December 2024 to identify randomized controlled trials that compared the efficacy of HFNC, COT and NIPPV in adult patients following CTS. A frequentist network meta-analysis was performed. Outcomes included reintubation rate, in-hospital mortality, ICU and hospital length of stay, pneumonia incidence, CPAP requirement, and PaCO2 levels.
Results
Eleven RCTs enrolling 1,664 patients were analyzed. There were no statistically significant differences in reintubation rates, in-hospital mortality, or CPAP requirements between HFNC and COT, NIPPV and COT, or NIPPV and HFNC. NIPPV significantly reduced ICU length of stay compared to both COT (MD –52.16 hours; 95% CI, –77.94 to –26.38) and HFNC (MD –41.99 hours; 95% CI, –67.69 to –16.28), and also shortened hospital length of stay compared to COT (MD –2.51 days; 95% CI, –4.82 to –0.21). Both HFNC and NIPPV were associated with a significantly lower incidence of pneumonia compared to COT (HFNC: OR 0.11; 95% CI, 0.01 to 0.91; NIPPV: OR 0.12; 95% CI, 0.01 to 0.97). In terms of PaCO2 reduction, both HFNC and NIPPV significantly lowered levels compared with COT (HFNC: MD –2.68 mmHg; 95% CI, –3.32 to –2.04; NIPPV: MD –1.61 mmHg; 95% CI, –2.26 to –0.96), with HFNC showing a greater reduction than NIPPV (MD 1.07 mmHg; 95% CI, 0.93 to 1.20).
Conclusion
In adult patients undergoing cardiothoracic surgery, the rates of reintubation and in-hospital mortality were similar across noninvasive respiratory support strategies. NIPPV may reduce ICU and hospital length of stay compared with HFNC and COT, while both HFNC and NIPPV may lower the incidence of pneumonia relative to COT. Although these findings support the use of HFNC or NIPPV over COT, the lack of significant differences in key clinical outcomes and overall low certainty of evidence underscores the need for further high-quality randomized trials to clarify their comparative effectiveness.
More abstracts on this topic:
Airway Opening Index is Associated with Return of Spontaneous Circulation in Swine and Humans with Cardiac Arrest
Bhandari Shiv, Coult Jason, Sharpe Zachary, Rea Thomas, Neumar Robert, Hsu Cindy, Counts Catherine, Sayre Michael, Johnson Nicholas
Attenuating Post-stroke Ischemia Reperfusion Injury: Establishing the Efficacy of Disodium Malonate in a Clinically Relevant Sheep ModelSorby-adams Annabel, Murphy Mike, Sharkey Jessica, Prag Hiran, Turner Renee, Skein Keziah, Guglietti Bianca, Pullan Caitlin, Williams Georgia, Krieg Thomas