Final ID: MP926
Prevalence and Outcomes of Antiphospholipid Antibodies in Patients with Peripheral Artery Disease
Background: Although antiphospholipid antibodies (aPL) are classically associated with excess risk of thrombosis in antiphospholipid syndrome (APS), emerging data suggest that aPLs may confer a prognostic role in patients with cardiovascular conditions who do not fulfill traditional research criteria for APS. We aimed to investigate the prevalence of aPL seropositivity among patients with peripheral artery disease (PAD) and to assess outcomes among those with and without aPL.
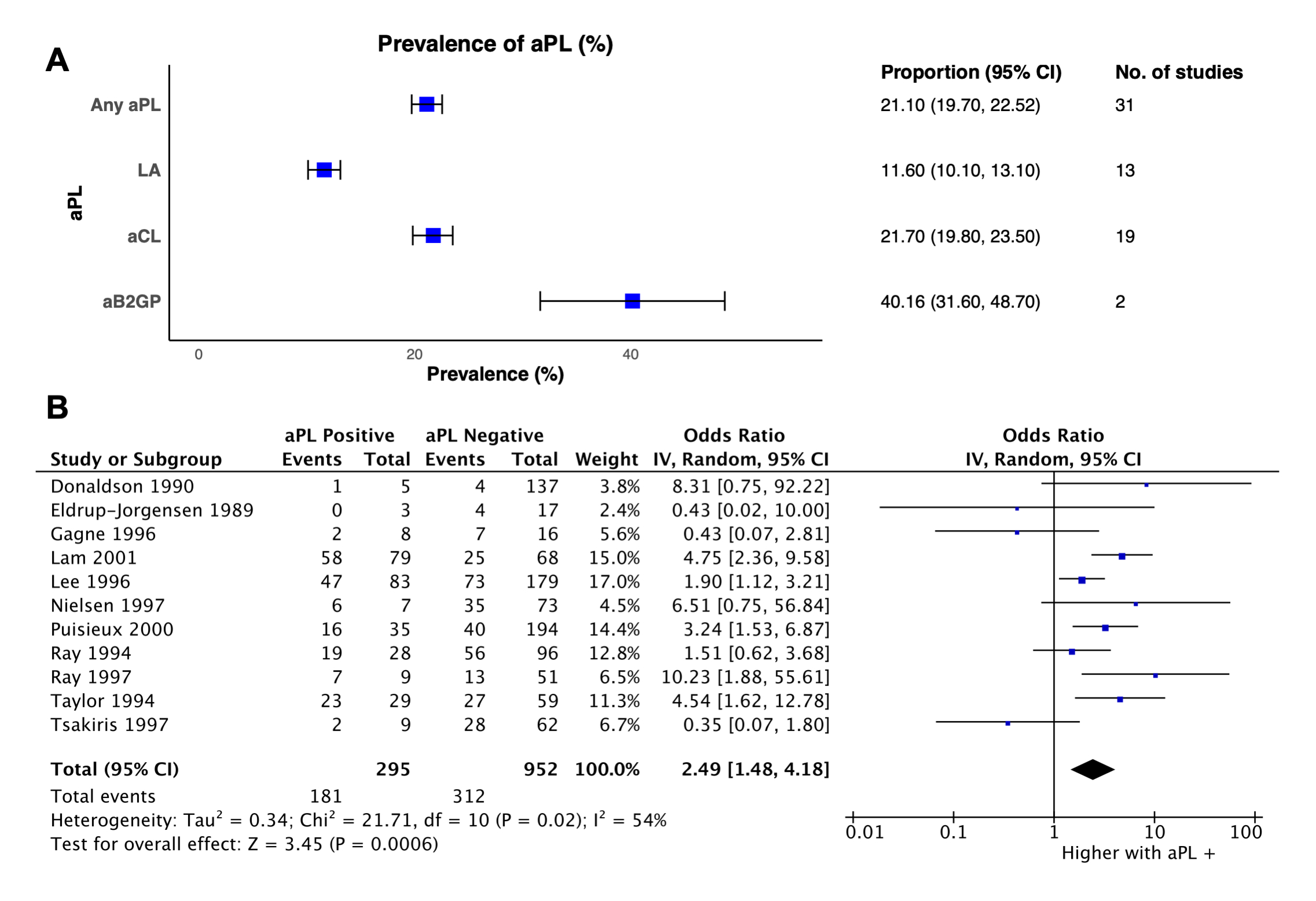
Methods: In this study, as part of a larger project (PROSPERO ID CRD420251047305), we systematically searched PubMed and Embase through 3/11/2025 to determine the pooled prevalence of aPL seropositivity among patients with PAD. Despite variation in PAD severity across studies, aPL testing occurred in unselected individuals (rather than by clinical suspicion). aPL positivity was defined as at least one single positive measurement for either anticardiolipin, anti-β2 glycoprotein, or lupus anticoagulant. For studies with longitudinal data available, we assessed a composite outcome of subsequent arterial thrombosis, revascularization failure, amputations, and death stratified by aPL seropositivity. Random-effects models with inverse weights were used to calculate pooled odds ratios (ORs).
Results: Among 2,890 records, we identified 31 studies assessing aPL prevalence and 11 evaluating clinical outcomes (3,364 total patients, mean age 58.6 years, 62.3% men). Seropositivity for at least one aPL was observed in 21.1% of patients with PAD (95% CI, 19.7%-22.5%). aPL seropositivity was associated with a significantly higher odds of the primary outcome (OR: 2.49, 95% CI 1.48-4.18) (Figure). Among patients who underwent revascularization, aPL seropositivity was associated with a higher odds of a failed revascularization procedure (OR: 2.72, 95% CI 1.49-4.98).
Conclusion: aPL seropositivity is present in approximately one-in-five patients with PAD and correlates with a subsequent risk of adverse clinical events. Whether early testing can help inform management strategies and improve outcomes requires further investigation.
- Watson, Nathan ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Goldhaber, Samuel ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Connors, Jean ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Uljon, Sacha ( Massachusetts General Hospital , Boston , Massachusetts , United States )
- Secemsky, Eric ( BIDMC , Boston , Massachusetts , United States )
- Lip, Gregory ( University of Liverpool , Liverpool , United Kingdom )
- Krumholz, Harlan ( Yale University , New Haven , Connecticut , United States )
- Knight, Jason ( University of Michigan , Ann Arbor , Michigan , United States )
- Cushman, Mary ( UNIVERSITY VERMONT , Colchester , Vermont , United States )
- Costenbader, Karen ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Piazza, Gregory ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Siddiqui, Saman Asad ( Harvard Medical School , Boston , Massachusetts , United States )
- Bikdeli, Behnood ( Brigham and Womens Hospital , Boston , Massachusetts , United States )
- Rashedi, Sina ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Pfeferman, Mariana ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Jimenez, David ( Hospital Ramón y Cajal and Universidad de Alcalá , Madrid , Spain )
- Monreal, Manuel ( UCAM University , Barcelona , Spain )
- Barnes, Geoffrey ( University of Michigan , Ann Arbor , Michigan , United States )
- Galli, Mattia ( Sapienza University of Rome , Rome , Italy )
- Weber, Brittany ( BRIGHAM AND WOMENS HOSPITAL , Boston , Massachusetts , United States )
Meeting Info:
Session Info:
Vascular Genetics, Genomics, and Risk Scores
Saturday, 11/08/2025 , 03:15PM - 04:30PM
Moderated Digital Poster Session
More abstracts on this topic:
Muller Matthew, Boothman Isabelle, Luttrell-williams Elliot, Xia Yuhe, Barrett Tessa, Ruggles Kelly, Berger Jeffrey
A Rare Case of Loeffler Endocarditis and Intracardiac Thrombus in the setting of FIP1L1-PDGFRA MutationShaik Aleesha, Pankayatselvan Varayini, Mazar Michael, Bokhoor Pooya
More abstracts from these authors:
Rashedi Sina, Hussain Mohamad, Mojibian Hamid, Goldhaber Samuel, Zhou Li, Yang Richard, Wang Liqin, Krumholz Harlan, Piazza Gregory, Bikdeli Behnood, Bukhari Syed, Krishnathasan Darsiya, Khairani Candrika, Bejjani Antoine, Pfeferman Mariana, Zarghami Mehrdad, Secemsky Eric, Rahaghi Farbod
Association Between Antiphospholipid Antibody and Ischemic Stroke: A Systematic Review and Meta-AnalysisWatson Nathan, Kanthi Yogen, Secemsky Eric, Connors Jean, Barnes Geoffrey, Goldhaber Samuel, Weitz Jeffrey, Costenbader Karen, Piazza Gregory, Krumholz Harlan, Cushman Mary, Bukhari Syed, Bikdeli Behnood, Rashedi Sina, Weber Brittany, Anderson Christopher, Elkind Mitchell, Pfeferman Mariana, Ujueta Francisco, Zarghami Mehrdad