Final ID: 4360623
Three Limbs Is Better Than Two: Weathering Electrical Storm with Veno-Arterial-Venous Extracorporeal Membrane Oxygenation
Abstract Body (Do not enter title and authors here): Description of Case
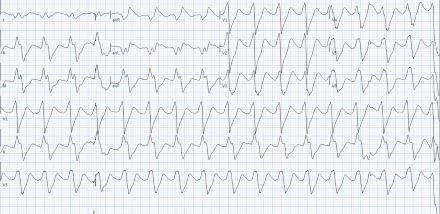
A 58 year old man with non-ischemic cardiomyopathy (LVEF 21%) secondary to presumed (non-biopsy proven) cardiac sarcoidosis on prednisone and infliximab status post CRT-D placement, recurrent admissions for VT, and CKD presented to the emergency room with right upper quadrant pain. Chest x-ray revealed right lower lobe pneumonia and he was started on broad-spectrum antibiotics. He was admitted to the ICU and rapidly developed severe acute hypoxemic respiratory failure requiring intubation, maximum ventilator support, and neuromuscular paralysis. He concomitantly developed severe shock requiring high doses of three vasopressors. In this setting, he had hemodynamically unstable runs of monomorphic VT treated with IV amiodarone and lidocaine. He suffered a VT arrest (Image 1), with rates below his device detection zone, and was externally defibrillated.
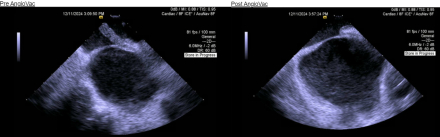
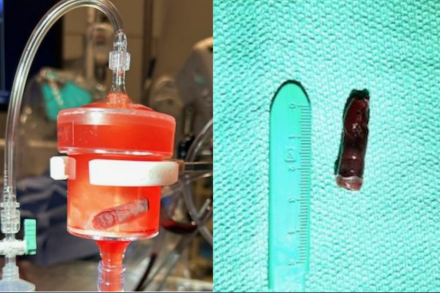
A Shock Team call was convened. He was cannulated on to veno-arterial-venous (V-AV) ECMO for refractory hypoxemia, VT and SCAI E cardiogenic shock. He underwent placement of an axillary Impella 5.5 for LV mechanical unloading. With time, his respiratory and circulatory status improved to the point of being able to liberate to V-V ECMO, which was subsequently decannulated, remaining on low-level Impella support throughout. His course was complicated by anuric renal failure requiring dialysis, mechanical device-related hemolysis, and a large, mobile right atrial thrombus. This clot appeared to be adherent to a PFO and was removed via AngioVac suction thrombectomy with live intra-cardiac echocardiographic guidance (Images 2, 3). Weaning of anti-arrhythmic drugs resulted in recurrence of VT. His back-up pacing rate was increased and he was deeply sedated, started on procainamide, and empirically treated for a sarcoidosis flare with pulse dose steroids, with residual breakthrough VT. Due to his ongoing infections, coagulopathy, multi-organ failure, and VT storm, he was deemed not a candidate for advanced therapies. He was transitioned to comfort-oriented care and passed away.
Discussion
This case illustrates the utility of a less conventional ECMO configuration in patients with combined cardiopulmonary failure, while also highlighting the challenge of treating VT storm in a patient with inflammatory cardiomyopathy and septic shock. Finally, we demonstrate the role for suction thrombectomy in extracting large, mobile intra-cardiac thrombi to prevent embolic phenomena.
A 58 year old man with non-ischemic cardiomyopathy (LVEF 21%) secondary to presumed (non-biopsy proven) cardiac sarcoidosis on prednisone and infliximab status post CRT-D placement, recurrent admissions for VT, and CKD presented to the emergency room with right upper quadrant pain. Chest x-ray revealed right lower lobe pneumonia and he was started on broad-spectrum antibiotics. He was admitted to the ICU and rapidly developed severe acute hypoxemic respiratory failure requiring intubation, maximum ventilator support, and neuromuscular paralysis. He concomitantly developed severe shock requiring high doses of three vasopressors. In this setting, he had hemodynamically unstable runs of monomorphic VT treated with IV amiodarone and lidocaine. He suffered a VT arrest (Image 1), with rates below his device detection zone, and was externally defibrillated.
A Shock Team call was convened. He was cannulated on to veno-arterial-venous (V-AV) ECMO for refractory hypoxemia, VT and SCAI E cardiogenic shock. He underwent placement of an axillary Impella 5.5 for LV mechanical unloading. With time, his respiratory and circulatory status improved to the point of being able to liberate to V-V ECMO, which was subsequently decannulated, remaining on low-level Impella support throughout. His course was complicated by anuric renal failure requiring dialysis, mechanical device-related hemolysis, and a large, mobile right atrial thrombus. This clot appeared to be adherent to a PFO and was removed via AngioVac suction thrombectomy with live intra-cardiac echocardiographic guidance (Images 2, 3). Weaning of anti-arrhythmic drugs resulted in recurrence of VT. His back-up pacing rate was increased and he was deeply sedated, started on procainamide, and empirically treated for a sarcoidosis flare with pulse dose steroids, with residual breakthrough VT. Due to his ongoing infections, coagulopathy, multi-organ failure, and VT storm, he was deemed not a candidate for advanced therapies. He was transitioned to comfort-oriented care and passed away.
Discussion
This case illustrates the utility of a less conventional ECMO configuration in patients with combined cardiopulmonary failure, while also highlighting the challenge of treating VT storm in a patient with inflammatory cardiomyopathy and septic shock. Finally, we demonstrate the role for suction thrombectomy in extracting large, mobile intra-cardiac thrombi to prevent embolic phenomena.
More abstracts on this topic:
GLP-1 Receptor Agonists and Mortality Outcomes in Patients with Left Ventricular Assist Devices: A Propensity-Matched Cohort Study from the TriNetX Global Network
Alkhatib Ahmad, Ahmed Mustafa, Jarrar Yaman, Nazzal Jamil, Al Shaikhli Mustafa, Abdallah Omar Mohammad, Abdulelah Ahmed, Eldawud Daoud, Almaadawy Omar, Alomari Laith
Evaluation of ACTION-ICU Score as a Predictor of Complications Requiring Intensive Care in a Mexican Cohort of Patients with Non-ST-Segment Elevation Myocardial InfarctionAlanis Naranjo Jose Martin, Rivera Hermosillo Julio Cesar, Villegas Mayoral Jose Evodio