Final ID: MP2553
Interleukin-1 Blockade for Rheumatic Fever Pericarditis in a Steroid-Intolerant Patient: A Case Report
Abstract Body (Do not enter title and authors here): Introduction:
In developed nations, acute rheumatic fever (ARF) is a rare cause of pancarditis, including pericarditis. Corticosteroids, though second-line agents for pericarditis, are frequently used to treat the cardiac and joint manifestations of ARF. Interleukin-1 (IL-1) inhibitors offer targeted therapy in recurrent idiopathic pericarditis, yet their role in ARF-related pericarditis remains undefined. We describe the application of IL-1 blockade to post-streptococcal, autoimmune-mediated pericarditis in a patient intolerant to corticosteroids.
Case Report:
A 38-year-old man with pre-diabetes, hyperlipidemia, and recent upper respiratory infection presented with acute right hip arthritis and elevated inflammatory markers (CRP 190.6 mg/L, ESR 108 mm/hr). Arthrocentesis yielded inflammatory synovial fluid without infection. Symptoms resolved with NSAIDs, prompting discharge.
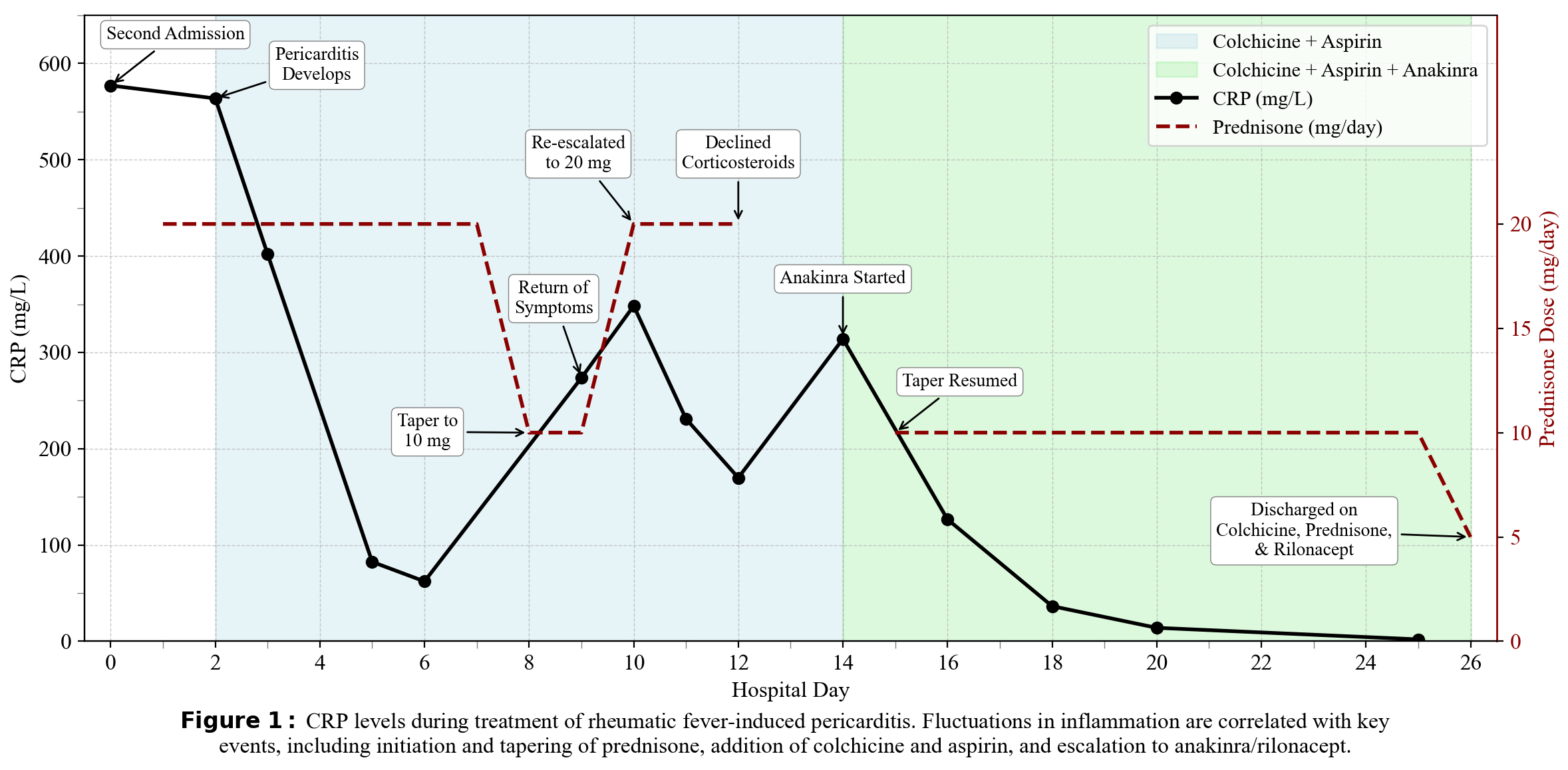
Four days later, he returned with high-grade fevers and diffuse polyarthralgia involving his wrists, hands, ankles, and feet. Exam uncovered migratory arthritis of the right hip and bilateral wrists. Labs showed CRP > 500 mg/L, high-titer antistreptolysin-O, leukocytosis, and acute kidney injury (AKI) with active urinary sediment. The presentation met Jones criteria for adult-onset ARF. Prednisone was started instead of NSAIDs for polyarthritis due to his AKI (figure 1).
Following renal recovery with supportive care, he developed pleuritic chest pain, a precordial friction rub, and a HS-troponin peak of 195 ng/L. ECG demonstrated diffuse ST elevations, PR depression, and Spodick’s sign. Echocardiography revealed a small-moderate pericardial effusion. Cardiac MRI showed no myocardial involvement but increased T2 signal and late gadolinium enhancement consistent with pericarditis. Colchicine and high-dose aspirin were initiated, which improved his chest pain and CRP (62 mg/L). However, prednisone taper triggered rebound chest pain, arthritis, and CRP elevation (348 mg/L). He declined a prolonged course of high-dose steroids due to anxiety and hyperglycemia. Anakinra was added, resulting in symptom relief and CRP reduction (2 mg/L). He was transitioned to weekly rilonacept at discharge.
Conclusion:
This case highlights IL-1 inhibition as a promising therapy in rare presentations of ARF-induced pericarditis, especially when corticosteroids are not tolerated. Using anakinra as a bridge to outpatient rilonacept may offer a targeted, steroid-sparing strategy in persistent pericarditis from ARF.
In developed nations, acute rheumatic fever (ARF) is a rare cause of pancarditis, including pericarditis. Corticosteroids, though second-line agents for pericarditis, are frequently used to treat the cardiac and joint manifestations of ARF. Interleukin-1 (IL-1) inhibitors offer targeted therapy in recurrent idiopathic pericarditis, yet their role in ARF-related pericarditis remains undefined. We describe the application of IL-1 blockade to post-streptococcal, autoimmune-mediated pericarditis in a patient intolerant to corticosteroids.
Case Report:
A 38-year-old man with pre-diabetes, hyperlipidemia, and recent upper respiratory infection presented with acute right hip arthritis and elevated inflammatory markers (CRP 190.6 mg/L, ESR 108 mm/hr). Arthrocentesis yielded inflammatory synovial fluid without infection. Symptoms resolved with NSAIDs, prompting discharge.
Four days later, he returned with high-grade fevers and diffuse polyarthralgia involving his wrists, hands, ankles, and feet. Exam uncovered migratory arthritis of the right hip and bilateral wrists. Labs showed CRP > 500 mg/L, high-titer antistreptolysin-O, leukocytosis, and acute kidney injury (AKI) with active urinary sediment. The presentation met Jones criteria for adult-onset ARF. Prednisone was started instead of NSAIDs for polyarthritis due to his AKI (figure 1).
Following renal recovery with supportive care, he developed pleuritic chest pain, a precordial friction rub, and a HS-troponin peak of 195 ng/L. ECG demonstrated diffuse ST elevations, PR depression, and Spodick’s sign. Echocardiography revealed a small-moderate pericardial effusion. Cardiac MRI showed no myocardial involvement but increased T2 signal and late gadolinium enhancement consistent with pericarditis. Colchicine and high-dose aspirin were initiated, which improved his chest pain and CRP (62 mg/L). However, prednisone taper triggered rebound chest pain, arthritis, and CRP elevation (348 mg/L). He declined a prolonged course of high-dose steroids due to anxiety and hyperglycemia. Anakinra was added, resulting in symptom relief and CRP reduction (2 mg/L). He was transitioned to weekly rilonacept at discharge.
Conclusion:
This case highlights IL-1 inhibition as a promising therapy in rare presentations of ARF-induced pericarditis, especially when corticosteroids are not tolerated. Using anakinra as a bridge to outpatient rilonacept may offer a targeted, steroid-sparing strategy in persistent pericarditis from ARF.
More abstracts on this topic:
Anti-inflammatory Agents and their Effect on Cardiovascular Disease: A Comprehensive Review of Literature
Malik Hamza, Harmouch Wissam, Mai Steven, Salehin Salman, Gilani Syed
Penicillin Prophylaxis and Adherence in Latent Rheumatic Heart Disease: Systematic Review and Metaanalysis of OutcomesSilva Pereira Claudio Cesar, Hartmann Rost Isabela, Pardo Isabele, Sevilhano Milanesi Gabriele, Dias Vilela Marcos Antonio