Final ID: Sa3019
Uncovering Cellular and Molecular Mechanisms in Fontan-Associated Liver Disease
Abstract Body (Do not enter title and authors here): Introduction:
Nearly 1 in 10,000 infants are born with a single ventricular heart, and these children must undergo the Fontan procedure to survive. As of 2020, an estimated 50,000 individuals are alive with a Fontan circulation. Although lifesaving, Fontan procedure is associated with several complications, including Fontan-associated liver disease (FALD). While elevated central venous pressure (CVP) appears to promote FALD, the cellular and molecular mechanisms involved in this unique liver disease are not well understood.
Methods:
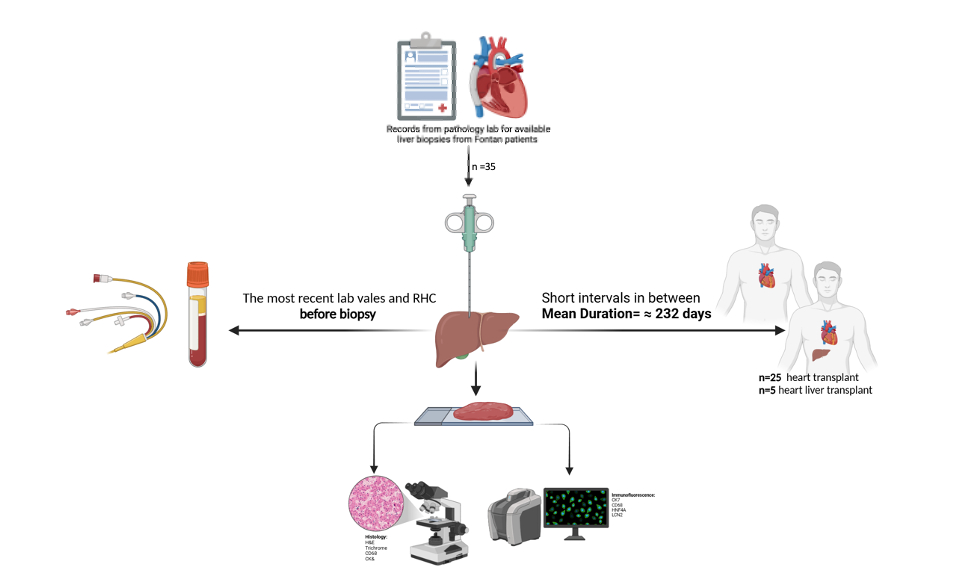
Liver biopsies from Fontan patients were collected at Washington University in St. Louis before heart transplant. Liver tissue was fixed in formalin and embedded in paraffin for H&E and Masson's trichrome staining. Immunohistochemistry, scRNA-seq, and immunofluorescence (IF) were performed. In our preclinical model, mice underwent pIVCL to mimic hepatic congestion and underwent IF, RNA analysis, and snRNA-seq.
Results:
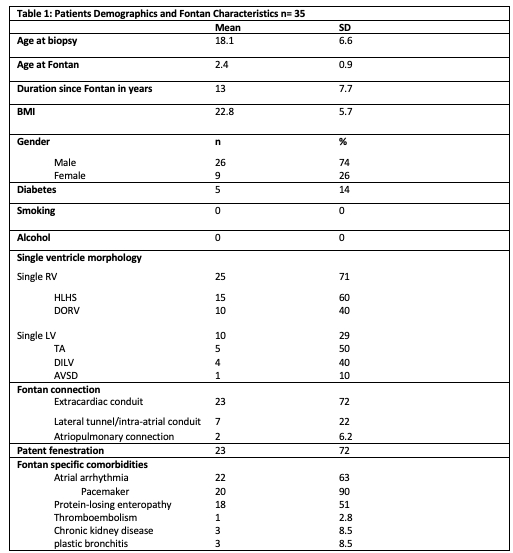
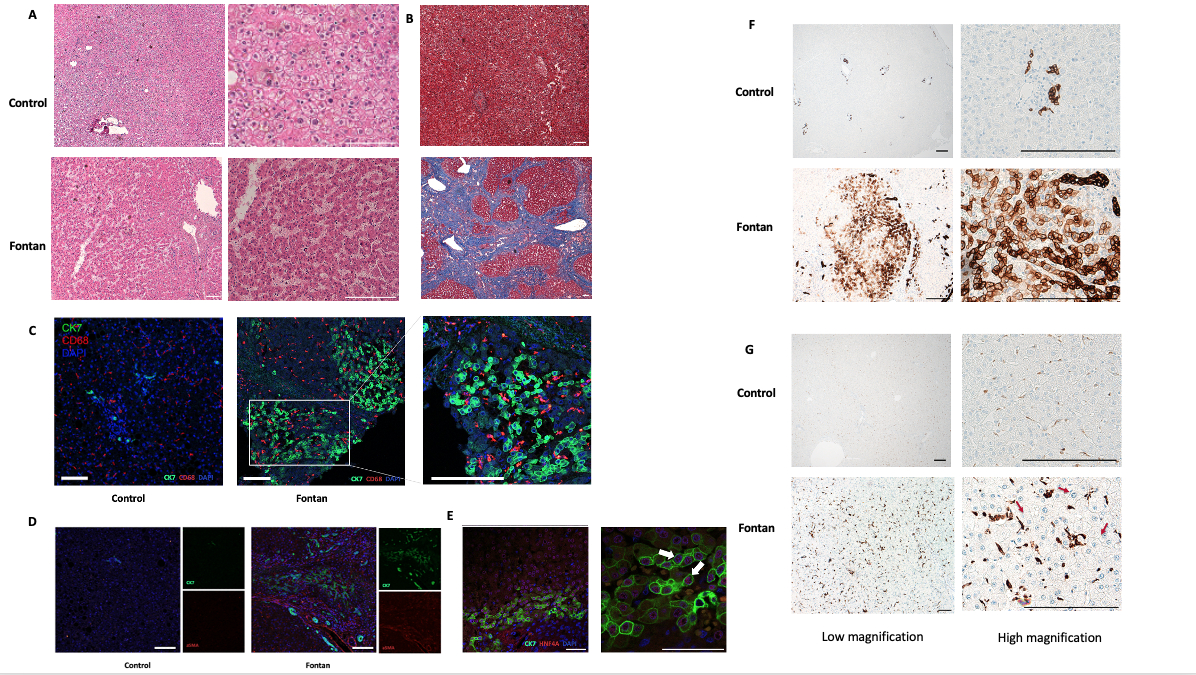
We recruited 35 patients with a mean age of 18.1 years (SD ±6.6) at the time of liver biopsy. The mean age at the time of the Fontan procedure was 2.4 years (SD ±0.9), with the average duration of Fontan circulation being 13 years. Regarding ventricular morphology, 25 patients (71%) had a single right ventricle, and 10 (29%) had a single left ventricle. The extracardiac conduit was the most common Fontan connection in 23 patients (72%). CVP was elevated in the superior vena cava (SVC) and Fontan conduit, with a mean of 18 mmHg (SD ±3.6). Liver function tests showed a median AST of 30.5 U/L (IQR 29.8), median ALT of 26.5 U/L (IQR 26.9), and median total bilirubin of 1.0 mg/dL (IQR 0.9). The mean APRI score was 0.58 (SD ±1.9), and MELD-XI was 10.2 (SD ±2.9). Fontan liver biopsies and liver sections from pIVCL mice showed sinusoidal dilatation, central hepatocyte dropout, and bridging fibrosis. Multiple areas of CK7-positive biliary metaplastic cells, which originated from HNF4α-positive hepatic progenitor cells, were identified. These areas colocalized with areas of CD68-positive aggregated macrophages and activated hepatic stellate cells (αSMA+). Using snRNA-seq in pIVCL and scRNA-seq in Fontan, we identified the cellular landscape in the cardiogenic liver disease.
Conclusions:
The interplay between sinusoidal congestion, macrophage activation, and biliary metaplasia in FALD implies a multifactorial pathogenesis that extends beyond passive venous congestion in cardiogenic liver diseases.
Nearly 1 in 10,000 infants are born with a single ventricular heart, and these children must undergo the Fontan procedure to survive. As of 2020, an estimated 50,000 individuals are alive with a Fontan circulation. Although lifesaving, Fontan procedure is associated with several complications, including Fontan-associated liver disease (FALD). While elevated central venous pressure (CVP) appears to promote FALD, the cellular and molecular mechanisms involved in this unique liver disease are not well understood.
Methods:
Liver biopsies from Fontan patients were collected at Washington University in St. Louis before heart transplant. Liver tissue was fixed in formalin and embedded in paraffin for H&E and Masson's trichrome staining. Immunohistochemistry, scRNA-seq, and immunofluorescence (IF) were performed. In our preclinical model, mice underwent pIVCL to mimic hepatic congestion and underwent IF, RNA analysis, and snRNA-seq.
Results:
We recruited 35 patients with a mean age of 18.1 years (SD ±6.6) at the time of liver biopsy. The mean age at the time of the Fontan procedure was 2.4 years (SD ±0.9), with the average duration of Fontan circulation being 13 years. Regarding ventricular morphology, 25 patients (71%) had a single right ventricle, and 10 (29%) had a single left ventricle. The extracardiac conduit was the most common Fontan connection in 23 patients (72%). CVP was elevated in the superior vena cava (SVC) and Fontan conduit, with a mean of 18 mmHg (SD ±3.6). Liver function tests showed a median AST of 30.5 U/L (IQR 29.8), median ALT of 26.5 U/L (IQR 26.9), and median total bilirubin of 1.0 mg/dL (IQR 0.9). The mean APRI score was 0.58 (SD ±1.9), and MELD-XI was 10.2 (SD ±2.9). Fontan liver biopsies and liver sections from pIVCL mice showed sinusoidal dilatation, central hepatocyte dropout, and bridging fibrosis. Multiple areas of CK7-positive biliary metaplastic cells, which originated from HNF4α-positive hepatic progenitor cells, were identified. These areas colocalized with areas of CD68-positive aggregated macrophages and activated hepatic stellate cells (αSMA+). Using snRNA-seq in pIVCL and scRNA-seq in Fontan, we identified the cellular landscape in the cardiogenic liver disease.
Conclusions:
The interplay between sinusoidal congestion, macrophage activation, and biliary metaplasia in FALD implies a multifactorial pathogenesis that extends beyond passive venous congestion in cardiogenic liver diseases.
More abstracts on this topic:
Acceptability and Feasibility Of A Digital Health Intervention For Adults with Congenital Heart Disease
Valente Joseph, Reardon Leigh, Moons Philip, Okumura Megumi, Gurvitz Michelle, Agarwal Anushree, Banala Keerthana, Buenrostro Karina, Alano Lindsay, Duan Rong, Parang Kim, Manyan Karina, Bravo-jaimes Katia, Norris Mark
A Case of Dilated Cardiomyopathy and Systemic Thromboembolism in a Young Patient on Testosterone Replacement TherapySabri Muhammad, Ijaz Naila, Nadeem Ramsha, Checchio Lucy, Riaz Faiza