Final ID: MP839
Left Ventricular Ejection Fraction as a Prognostic Marker Across Gradient and Flow Subtypes in patients with severe aortic stenosis undergoing SAVR or TAVR: Insights from CURRENT AS Registry 2
Abstract Body (Do not enter title and authors here): Background
The prognostic significance of left ventricular ejection fraction (LVEF) has been reported in patients with severe aortic stenosis (AS), but remains inconclusive in those undergoing surgical (SAVR) or transcatheter aortic valve replacement (TAVR). The recent ACC/AHA guidelines introduced 60% as a new LVEF threshold for intervention in asymptomatic patients, in addition to the traditional cut-off of 50%. The study aimed to evaluate the association between pre-procedural LVEF and long-term clinical outcomes in patients undergoing either SAVR or TAVR.
Methods
Among 3,369 patients with severe AS enrolled in the CURRENT AS Registry 2, we analyzed 1,742 patients who underwent SAVR (n=594), and TAVR (n=1,148), based on the initial treatment strategy. We assessed the impact of pre-procedural LVEF and long-term outcomes. The primary outcome was defined as a composite of all-cause death or hospitalization for heart failure (HHF). Sensitivity analyses were performed according to AS subtypes, including high-gradient (mean pressure gradient [mPG] >40 mmHg) vs. low-gradient (mPG <40 mmHg), and normal-flow (stroke volume index [SVi] >35 ml) vs low-flow status (SVi <35 ml).
Result
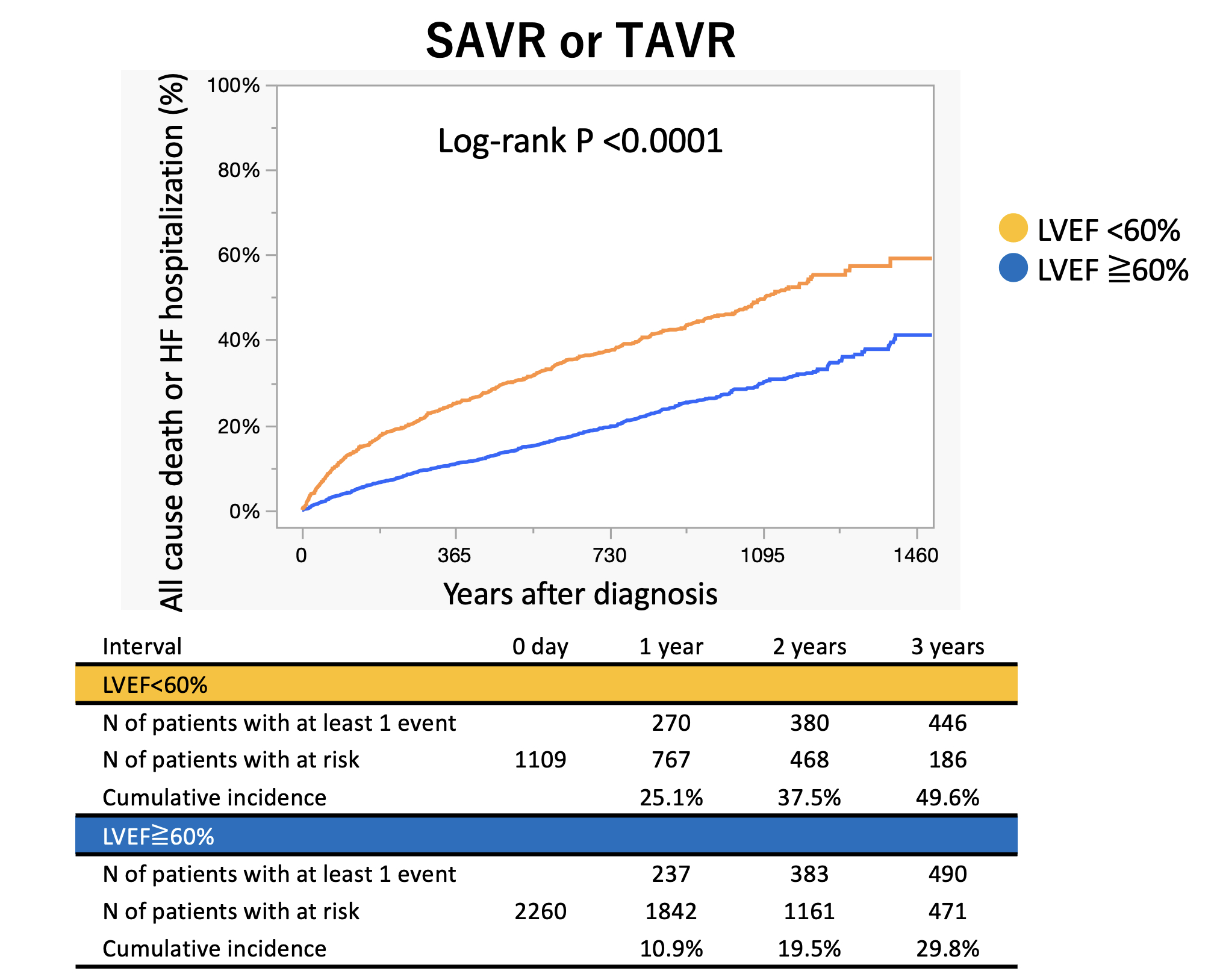
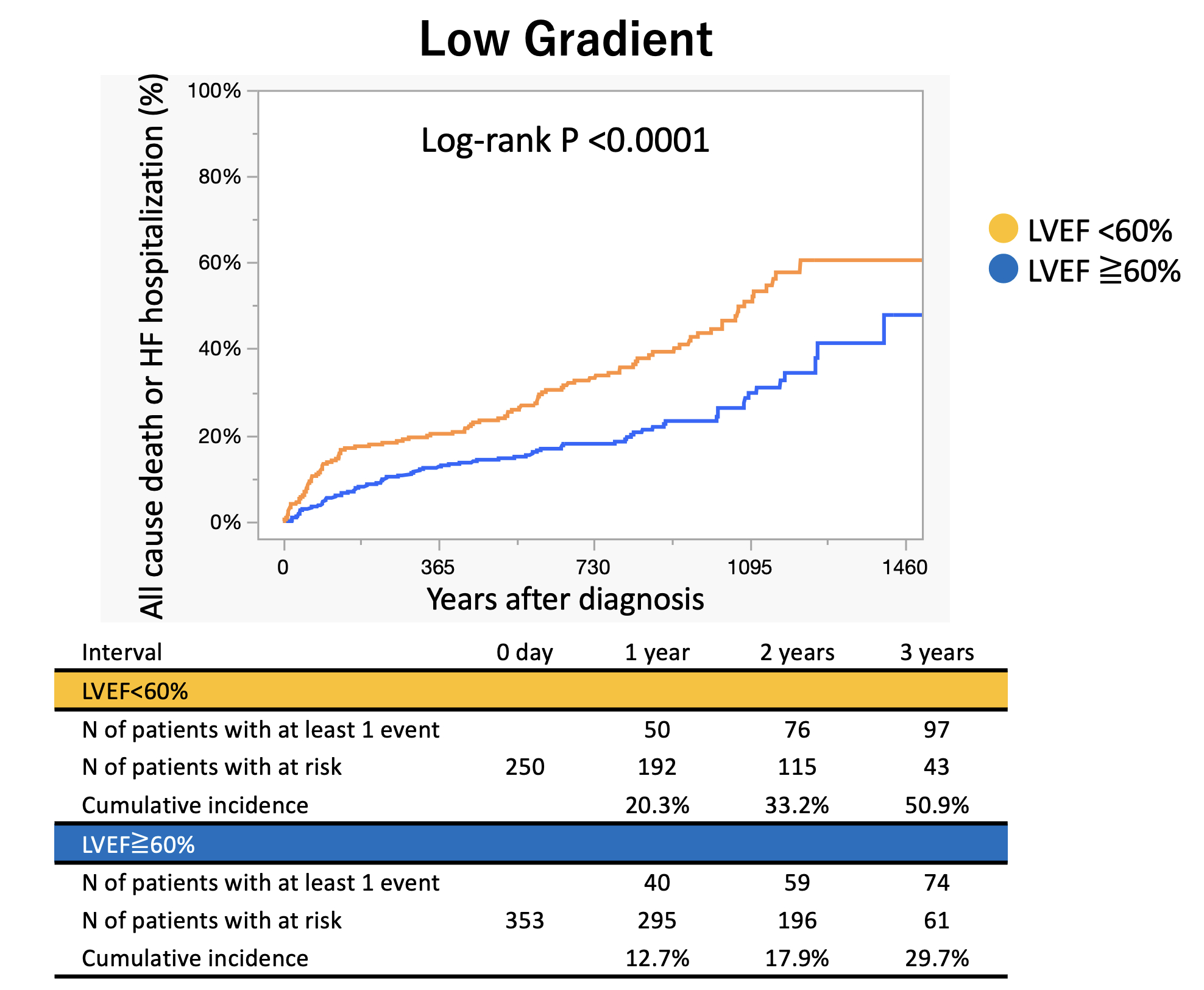
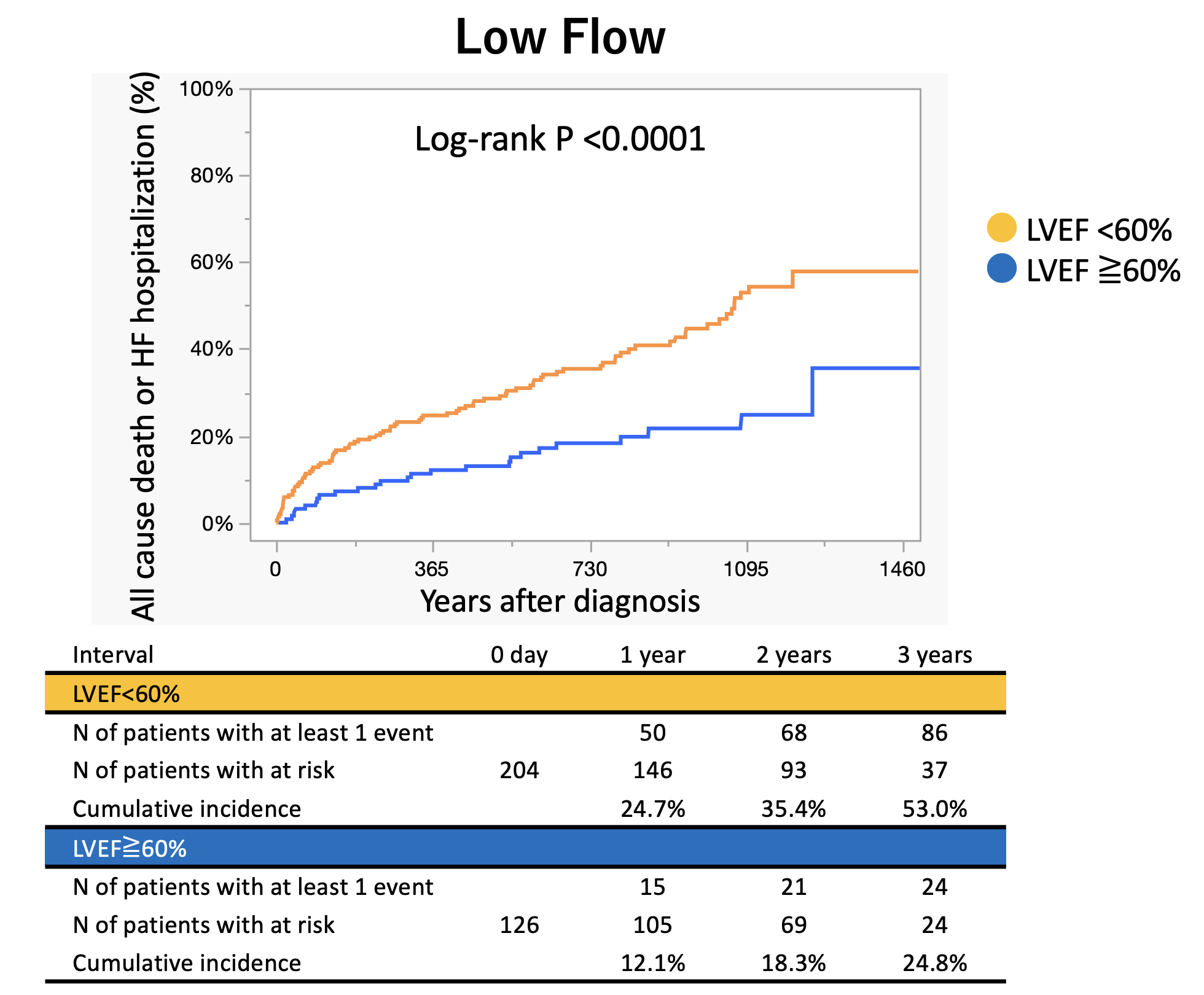
The mean age was 80.8 ± 8.1 years, and 40% were male. The mean pre-procedural LVEF was 60.7 ± 11.2%. During the median follow-up of 2.1 [interquartile range: 1.3-2.9] years, 379 primary outcome measures were observed (270 deaths and 164 HHF). Receiver operating characteristic curve analysis identified an optimal LVEF cutoff of 59.3% for predicting the primary outcome. Patients with LVEF<60% had significantly higher rates of the primary outcome, even after adjustment for confounders (adjusted hazard ratio [HR]: 1.50, 95% confidence interval [CI]: 1.20-1.88, p<0.001). This association remained consistent across subgroups, including low-gradient (adjusted HR: 1.88, 95% CI: 1.35-2.62, p<0.001), normal-flow (adjusted HR: 1.95, 95% CI: 1.16-3.27, p=0.012) and low-flow status (adjusted HR: 1.44, 95% CI: 1.11-1.87, p=0.007), but not for high-gradient (adjusted HR: 1.23, 95% CI: 0.90-1.68, p=0.20).
Conclusion
Pre-procedural LVEF was significantly associated with increased risk of adverse events following TAVR or SAVR. This association remained consistent across subgroups such as low-gradient AS and low-flow AS, supporting LVEF as a robust prognostic marker in patients with AS.
The prognostic significance of left ventricular ejection fraction (LVEF) has been reported in patients with severe aortic stenosis (AS), but remains inconclusive in those undergoing surgical (SAVR) or transcatheter aortic valve replacement (TAVR). The recent ACC/AHA guidelines introduced 60% as a new LVEF threshold for intervention in asymptomatic patients, in addition to the traditional cut-off of 50%. The study aimed to evaluate the association between pre-procedural LVEF and long-term clinical outcomes in patients undergoing either SAVR or TAVR.
Methods
Among 3,369 patients with severe AS enrolled in the CURRENT AS Registry 2, we analyzed 1,742 patients who underwent SAVR (n=594), and TAVR (n=1,148), based on the initial treatment strategy. We assessed the impact of pre-procedural LVEF and long-term outcomes. The primary outcome was defined as a composite of all-cause death or hospitalization for heart failure (HHF). Sensitivity analyses were performed according to AS subtypes, including high-gradient (mean pressure gradient [mPG] >40 mmHg) vs. low-gradient (mPG <40 mmHg), and normal-flow (stroke volume index [SVi] >35 ml) vs low-flow status (SVi <35 ml).
Result
The mean age was 80.8 ± 8.1 years, and 40% were male. The mean pre-procedural LVEF was 60.7 ± 11.2%. During the median follow-up of 2.1 [interquartile range: 1.3-2.9] years, 379 primary outcome measures were observed (270 deaths and 164 HHF). Receiver operating characteristic curve analysis identified an optimal LVEF cutoff of 59.3% for predicting the primary outcome. Patients with LVEF<60% had significantly higher rates of the primary outcome, even after adjustment for confounders (adjusted hazard ratio [HR]: 1.50, 95% confidence interval [CI]: 1.20-1.88, p<0.001). This association remained consistent across subgroups, including low-gradient (adjusted HR: 1.88, 95% CI: 1.35-2.62, p<0.001), normal-flow (adjusted HR: 1.95, 95% CI: 1.16-3.27, p=0.012) and low-flow status (adjusted HR: 1.44, 95% CI: 1.11-1.87, p=0.007), but not for high-gradient (adjusted HR: 1.23, 95% CI: 0.90-1.68, p=0.20).
Conclusion
Pre-procedural LVEF was significantly associated with increased risk of adverse events following TAVR or SAVR. This association remained consistent across subgroups such as low-gradient AS and low-flow AS, supporting LVEF as a robust prognostic marker in patients with AS.
More abstracts on this topic:
A Remedy for the Heart and the Hemoglobin: Improvement in Anemia Post Transcatheter Aortic Valve Replacement
Matta Raghav, Roy Aanya, Hammad Bayan, Draffen Arvind, Natsheh Zachary, Tiu Daniel, Tiu David, Salem Edward, Balami Jesse, Kalagara Swetha, Gupta Neil, Uraizee Omar, Sahgal Savina, Mishra Atreya, Ene Adriana, Hattab Aleyah, Arora Aarushi, Sufyaan Humam, Dau Trang, Silberstein Jonathan, Yu Julia, Torres Kayla, Seshadri Suhas, Navarro Laura, Singam Manisha, Ismail Mariam, Rana Riya, Habeel Samer, Liu Simon, Chaganti Srinidhi, Gurbuxani Vidur, Dwyer Kaluzna Stephanie, Groo Vicki, Carlson Andrew, Shroff Adhir, Bhayani Siddharth, Khan Azmer, Bhattaram Rohan, Zhang Runze, Shah Pal
Cardiomyocyte TRPV4 Deletion Mitigates Adverse Cardiac Remodeling Via Modulation of Protein Kinase G signalingKatari Venkatesh, Dalal Kesha, Kondapalli Narendra, Paruchuri Sailaja, Thodeti Charles