Final ID: MP1266
Ethnic Disparities in Post-Stroke Antihypertensive Therapy Intensification: Insights from the National Inpatient Sample (2018–2023)
Abstract Body (Do not enter title and authors here): Background: Hypertension management is critical to preventing recurrent stroke, yet racial and ethnic disparities in post-stroke antihypertensive therapy intensification remain underexplored. This study examines the rates of antihypertensive therapy intensification in Hispanic versus Non-Hispanic stroke patients using data from the National Inpatient Sample (NIS).
Objective: To evaluate differences in antihypertensive therapy intensification at hospital discharge among Hispanic and Non-Hispanic stroke patients, and to assess associated clinical outcomes using data from the National Inpatient Sample.
Methods: We performed a retrospective cohort study using NIS data from 2018 to 2023, identifying adults (≥18 years) hospitalized with ischemic or hemorrhagic stroke based on ICD-10 codes. Antihypertensive therapy intensification, defined as the addition of a new agent or a dose increase at discharge, was determined using discharge medication profiles and pharmacy billing data. Patients discharged to hospice or who were deceased during the index hospitalization were excluded.
The primary outcome was therapy intensification at discharge. Secondary outcomes included 30-day readmission for recurrent stroke and 90-day blood pressure control (<140/90 mmHg), based on linked follow-up data. Chi-square tests assessed group differences, and multivariable logistic regression was used to estimate adjusted odds ratios (aOR) for therapy intensification, controlling for demographic, clinical, and hospital-level variables. Statistical significance was set at p < 0.05.
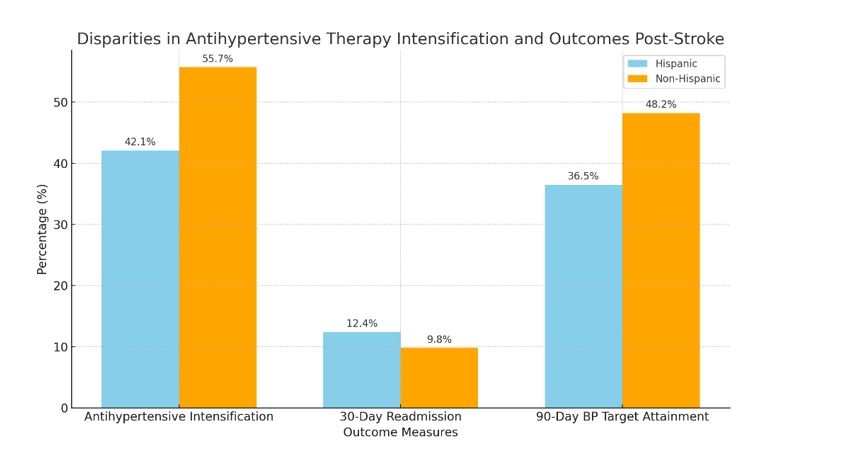
Results: Among 12,450 stroke patients, 3,780 (30.3%) were Hispanic. Antihypertensive therapy intensification occurred in 42.1% of Hispanic patients compared to 55.7% of Non-Hispanic patients (p < 0.05). Hispanic patients had a 23% lower likelihood of therapy intensification at discharge (OR: 0.77, 95% CI: 0.69-0.86). Thirty-day readmission rates for recurrent stroke were higher in Hispanic patients (12.4% vs. 9.8%, p < 0.01). Target blood pressure attainment at 90 days was achieved in 36.5% of Hispanic patients compared to 48.2% of Non-Hispanic patients (p < 0.05).
Conclusion: Hispanic patients post-stroke are less likely to receive antihypertensive therapy intensification at discharge, potentially contributing to higher readmission rates and poorer blood pressure control. These findings underscore the need for targeted interventions to mitigate disparities in cardiovascular care.
Objective: To evaluate differences in antihypertensive therapy intensification at hospital discharge among Hispanic and Non-Hispanic stroke patients, and to assess associated clinical outcomes using data from the National Inpatient Sample.
Methods: We performed a retrospective cohort study using NIS data from 2018 to 2023, identifying adults (≥18 years) hospitalized with ischemic or hemorrhagic stroke based on ICD-10 codes. Antihypertensive therapy intensification, defined as the addition of a new agent or a dose increase at discharge, was determined using discharge medication profiles and pharmacy billing data. Patients discharged to hospice or who were deceased during the index hospitalization were excluded.
The primary outcome was therapy intensification at discharge. Secondary outcomes included 30-day readmission for recurrent stroke and 90-day blood pressure control (<140/90 mmHg), based on linked follow-up data. Chi-square tests assessed group differences, and multivariable logistic regression was used to estimate adjusted odds ratios (aOR) for therapy intensification, controlling for demographic, clinical, and hospital-level variables. Statistical significance was set at p < 0.05.
Results: Among 12,450 stroke patients, 3,780 (30.3%) were Hispanic. Antihypertensive therapy intensification occurred in 42.1% of Hispanic patients compared to 55.7% of Non-Hispanic patients (p < 0.05). Hispanic patients had a 23% lower likelihood of therapy intensification at discharge (OR: 0.77, 95% CI: 0.69-0.86). Thirty-day readmission rates for recurrent stroke were higher in Hispanic patients (12.4% vs. 9.8%, p < 0.01). Target blood pressure attainment at 90 days was achieved in 36.5% of Hispanic patients compared to 48.2% of Non-Hispanic patients (p < 0.05).
Conclusion: Hispanic patients post-stroke are less likely to receive antihypertensive therapy intensification at discharge, potentially contributing to higher readmission rates and poorer blood pressure control. These findings underscore the need for targeted interventions to mitigate disparities in cardiovascular care.
More abstracts on this topic:
A Multi-Center Clinic Site Comparison of Patient-level factors Affecting Oral Anticoagulation Prescription for Atrial Fibrillation
Iqbal Fatima, Hoang Kenneth, Chiadika Simbo
Association of Workflow Metrics with Functional Outcomes in the SELECT2 trialJabbour Pascal, Sitton Clark, Churilov Leonid, Hill Michael, Ribo Marc, Campbell Bruce, Gandhi Chirag, Tjoumakaris Stavropoula, Sarraj Amrou, Al-mufti Fawaz, Hassan Ameer, Abraham Michael, Hussain Shazam, Ortega-gutierrez Santiago, Chen Michael, Pujara Deep, Johns Hannah Tabitha