Final ID: MP1508
The Impact of Inflammatory Cumulative Burden on the Risk of Metabolic Dysfunction-Associated Steatotic Liver Disease
Abstract Body (Do not enter title and authors here): Background:
Metabolic dysfunction-associated steatotic liver disease (MASLD) has been a significant global public health challenge, with chronic inflammation playing a central role in its pathogenesis. The cumulative impact of long-term low-grade inflammation, defined as inflammatory cumulative burden, on MASLD risk remains unknown.
Methods:
This prospective cohort study analyzed 2,126 adults without baseline MASLD from the Tongzhou cohort study (ClinicalTrials.gov Identifier: NCT05156580), who underwent annual health examinations from 2016 to 2019 at Yongshun Community Health Center in Beijing, China. Integrated inflammatory cumulative burden was quantified using a composite score (range: 5–20) derived from five traditional inflammatory biomarkers: platelet count, neutrophil count, lymphocyte count, monocyte count, and C-reactive protein (CRP). Multivariable Cox proportional hazards regression assessed associations between the both integrated and individual inflammatory cumulative burden and MASLD risk. Restricted cubic spline (RCS) analyses evaluated dose-response relationships, and subgroup analyses tested interactions by sex, age, and body mass index (BMI).
Results:
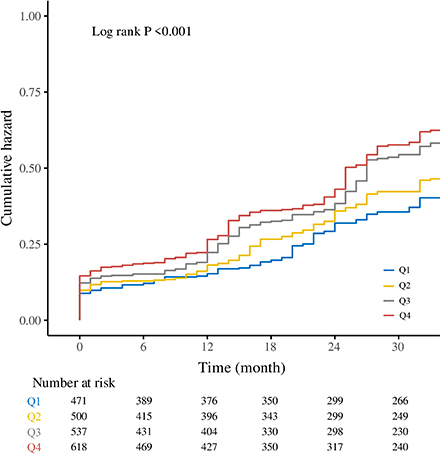
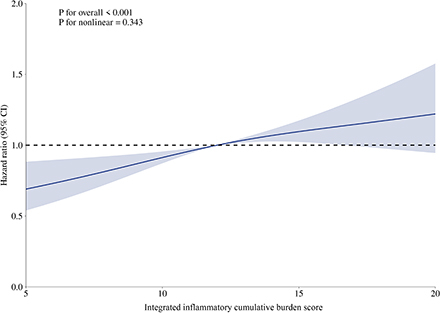
During a median follow-up of 27 months, higher inflammatory burden scores were associated with increased cumulative MASLD risk. Each 1-standard deviation (SD) increase in the integrated score elevated MASLD risk by 16% (adjusted HR, 1.16; 95% CI, 1.08–1.23; P < 0.001), with the highest quartile (Q4) exhibiting a 39% higher risk than the lowest (Q1) (adjusted HR, 1.39; 95% CI, 1.16–1.68; P < 0.001). RCS analysis confirmed a linear positive trend between the integrated score and MASLD risk (P for overall trend < 0.001; P for nonlinearity = 0.343). The cumulative burden of individual inflammatory markers was positively correlated with the MASLD risk. Subgroup analyses revealed no significant interactions by sex, age, or BMI (all P for interaction > 0.05).
Conclusion:
Inflammatory cumulative burden represents a risk factor for MASLD onset. Higher integrated and individual inflammatory cumulative burden is independently associated with increased MASLD risk. These findings enhance our understanding of MASLD pathogenesis and offer guidance for early identification, prevention, and intervention, highlighting the need to reduce chronic inflammation in prevention strategies.
Metabolic dysfunction-associated steatotic liver disease (MASLD) has been a significant global public health challenge, with chronic inflammation playing a central role in its pathogenesis. The cumulative impact of long-term low-grade inflammation, defined as inflammatory cumulative burden, on MASLD risk remains unknown.
Methods:
This prospective cohort study analyzed 2,126 adults without baseline MASLD from the Tongzhou cohort study (ClinicalTrials.gov Identifier: NCT05156580), who underwent annual health examinations from 2016 to 2019 at Yongshun Community Health Center in Beijing, China. Integrated inflammatory cumulative burden was quantified using a composite score (range: 5–20) derived from five traditional inflammatory biomarkers: platelet count, neutrophil count, lymphocyte count, monocyte count, and C-reactive protein (CRP). Multivariable Cox proportional hazards regression assessed associations between the both integrated and individual inflammatory cumulative burden and MASLD risk. Restricted cubic spline (RCS) analyses evaluated dose-response relationships, and subgroup analyses tested interactions by sex, age, and body mass index (BMI).
Results:
During a median follow-up of 27 months, higher inflammatory burden scores were associated with increased cumulative MASLD risk. Each 1-standard deviation (SD) increase in the integrated score elevated MASLD risk by 16% (adjusted HR, 1.16; 95% CI, 1.08–1.23; P < 0.001), with the highest quartile (Q4) exhibiting a 39% higher risk than the lowest (Q1) (adjusted HR, 1.39; 95% CI, 1.16–1.68; P < 0.001). RCS analysis confirmed a linear positive trend between the integrated score and MASLD risk (P for overall trend < 0.001; P for nonlinearity = 0.343). The cumulative burden of individual inflammatory markers was positively correlated with the MASLD risk. Subgroup analyses revealed no significant interactions by sex, age, or BMI (all P for interaction > 0.05).
Conclusion:
Inflammatory cumulative burden represents a risk factor for MASLD onset. Higher integrated and individual inflammatory cumulative burden is independently associated with increased MASLD risk. These findings enhance our understanding of MASLD pathogenesis and offer guidance for early identification, prevention, and intervention, highlighting the need to reduce chronic inflammation in prevention strategies.
More abstracts on this topic:
Aging-Associated Protein Medin Induces Human Coronary Artery Endothelial Proinflammatory and Prothrombotic Activation
Karamanova Nina, Morrow Kaleb, Maerivoet Alana, Madine Jillian, Li Ming, Migrino Raymond
A human cardiomyocyte model of CD36 haploinsufficiency uncovers fatty acid oxidation deficits driving dilated cardiomyopathyAl Sayed Zeina, Klattenhoff Carla, Aragam Krishna, Ellinor Patrick, Willcox Jon, Zheng Alice, Koledova Vera, Srivastava Salil, Yin Xiaofei, Chaffin Mark, Rigaud Vagner, Kovacs-bogdan Erika