Final ID: Mo3144
Prognostic Impact of Heart Failure in Acute Limb Ischemia: A Propensity Score Matched Analysis of National Inpatient Sample Data (2016–2020)
Abstract Body (Do not enter title and authors here): Background: Heart failure (HF) is a known risk factor for adverse outcomes in cardiovascular diseases, but its impact on acute limb ischemia (ALI) outcomes remains underexplored. This study evaluates the effect of HF on inpatient mortality, amputation rates, length of stay (LOS), and hospital costs in ALI patients using a nationally representative cohort.
Methods: We queried the National Inpatient Sample (2016–2020) and identified 44,913 ALI-related admissions. After excluding patients <18 years and records with missing key variables, 37,026 adult cases remained, of which 8,489 had a diagnosis of HF. Propensity score matching (PSM; 1:1 nearest neighbor) was performed using 35 clinical and demographic variables, yielding a final matched cohort of 16,978 patients (8,489 with HF and 8,489 without HF). Primary outcomes were inpatient mortality and major amputation. Secondary outcomes included LOS and total hospitalization cost (TOTCHG). Logistic regression assessed binary outcomes, Wilcoxon rank-sum tests compared continuous variables, and Kaplan-Meier curves estimated survival differences.
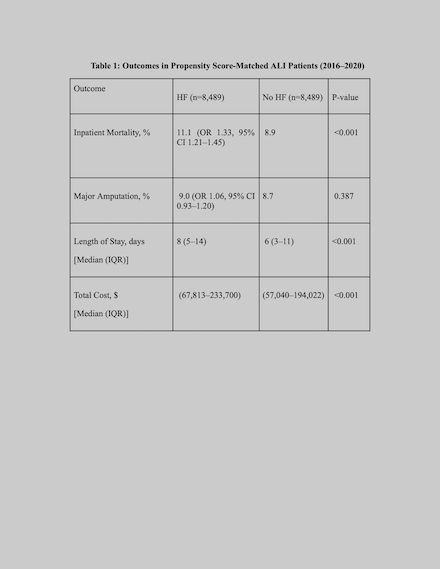
Results: In the matched cohort of 16,978 ALI patients (mean age 69.5 years, 46.8% female), racial/ethnic composition was predominantly White (72.3%), followed by Black (14.6%), Hispanic (8.0%), Asian or Pacific Islander (1.6%), Native American (0.6%), and Other (2.9%). Patients with HF had significantly higher inpatient mortality than those without HF (11.1% vs. 8.9%; OR 1.33, 95% CI 1.21–1.45, p < 0.001). Major amputation rates were similar between groups (9.0% vs. 8.7%; OR 1.06, 95% CI 0.93–1.20, p = 0.387). HF patients had a longer median LOS (8 days [IQR: 5–14] vs. 6 days [IQR: 3–11]; p < 0.001) and higher median total hospitalization cost ($111,794 [IQR: $67,813–$233,700] vs. $98,022 [IQR: $57,040–$194,022]; p = <0.001). Kaplan-Meier survival analysis showed a trend toward worse inpatient survival in the HF group (log-rank p = 0.055).
Conclusions: In patients hospitalized with ALI, HF is associated with significantly increased inpatient mortality, longer hospital stays, and higher costs. These findings highlight the critical need for proactive HF management in ALI to reduce mortality and healthcare burden.
Methods: We queried the National Inpatient Sample (2016–2020) and identified 44,913 ALI-related admissions. After excluding patients <18 years and records with missing key variables, 37,026 adult cases remained, of which 8,489 had a diagnosis of HF. Propensity score matching (PSM; 1:1 nearest neighbor) was performed using 35 clinical and demographic variables, yielding a final matched cohort of 16,978 patients (8,489 with HF and 8,489 without HF). Primary outcomes were inpatient mortality and major amputation. Secondary outcomes included LOS and total hospitalization cost (TOTCHG). Logistic regression assessed binary outcomes, Wilcoxon rank-sum tests compared continuous variables, and Kaplan-Meier curves estimated survival differences.
Results: In the matched cohort of 16,978 ALI patients (mean age 69.5 years, 46.8% female), racial/ethnic composition was predominantly White (72.3%), followed by Black (14.6%), Hispanic (8.0%), Asian or Pacific Islander (1.6%), Native American (0.6%), and Other (2.9%). Patients with HF had significantly higher inpatient mortality than those without HF (11.1% vs. 8.9%; OR 1.33, 95% CI 1.21–1.45, p < 0.001). Major amputation rates were similar between groups (9.0% vs. 8.7%; OR 1.06, 95% CI 0.93–1.20, p = 0.387). HF patients had a longer median LOS (8 days [IQR: 5–14] vs. 6 days [IQR: 3–11]; p < 0.001) and higher median total hospitalization cost ($111,794 [IQR: $67,813–$233,700] vs. $98,022 [IQR: $57,040–$194,022]; p = <0.001). Kaplan-Meier survival analysis showed a trend toward worse inpatient survival in the HF group (log-rank p = 0.055).
Conclusions: In patients hospitalized with ALI, HF is associated with significantly increased inpatient mortality, longer hospital stays, and higher costs. These findings highlight the critical need for proactive HF management in ALI to reduce mortality and healthcare burden.
More abstracts on this topic:
A New Analytical Approach for Noninvasive Reconstruction of the Entire Left Ventricular Pressure Waveform in Myocardial Ischemia and Infarction
Bilgi Coskun, Li Jiajun, Alavi Rashid, Dai Wangde, Matthews Ray, Kloner Robert, Pahlevan Niema
9-Year Longitudinal Assessment of the 12-lead Electrocardiogram of Volunteer FirefightersBae Alexander, Dzikowicz Dillon, Lai Chi-ju, Brunner Wendy, Krupa Nicole, Carey Mary, Tam Wai Cheong, Yu Yichen