Final ID: Su3021
Trends in United States Mortality Among Patients with Atrial Fibrillation/Flutter-Induced Heart Failure (1999–2024): Disparities by Gender, Race/Ethnicity and Region
Abstract Body (Do not enter title and authors here): Background:
Atrial fibrillation (AF) and heart failure (HF) are prevalent cardiovascular disorders that frequently co-occur, exacerbating each other's effects and resulting in adverse clinical outcomes. Despite the well-established association between these conditions, there is a paucity of research examining AF/atrial flutter (AFL) as direct contributors to HF-related mortality across various demographics and regions within the United States
Hypothesis:
This study aims to investigate the patterns of AF/AFL-related HF mortality in the U.S. from 1999 to 2024, stratified by age, gender, race/ethnicity, urban-rural classification, and geographic region.
Methods:
A retrospective analysis was conducted utilizing data from the Centers for Disease Control and Prevention's Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database. Mortality data were extracted from death certificates that identified AF/AFL related HF as a primary or contributing cause of death (ICD-10 codes I11.0, I13.0, I13.2, I48 and I50). Age-adjusted mortality rates (AAMRs) per 100,000 individuals were calculated, and annual percentage changes (APC) were assessed using Joinpoint regression.
Results:
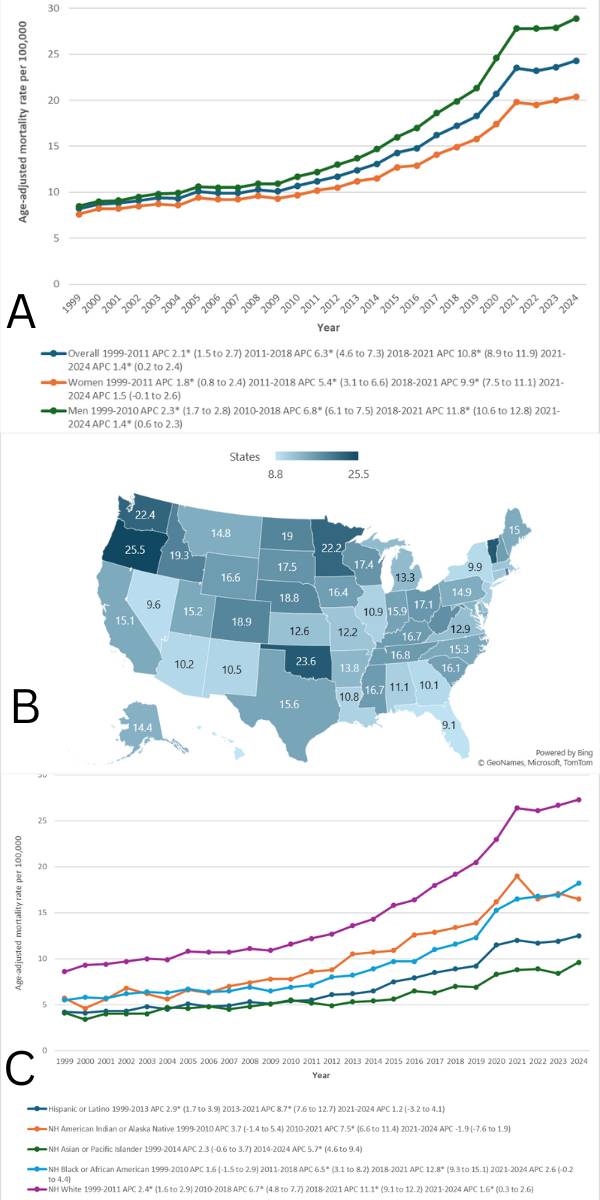
From 1999 to 2024, 1,307,809 deaths in the United States were attributed to atrial fibrillation/flutter-related heart failure (AF/AFL-HF). The age-adjusted mortality rate (AAMR) rose significantly from 8.2 to 24.3 per 100,000. Males consistently had higher AAMRs than females (15.7 vs. 12.3). Racial disparities were evident, with non-Hispanic Whites having the highest cumulative AAMR (15.1), and non-Hispanic Asians/Pacific Islanders the lowest (5.7). Geographic differences were also prominent: Oregon recorded the highest state-level AAMR (25.5), while Hawaii had the lowest (8.8). Regionally, the West (15.3) and Midwest (14.9) had the highest cumulative AAMRs. Place-of-death trends showed a shift toward home deaths, which became the most common location by 2024. Although AAMRs increased sharply from 2010 to 2021 across most subgroups, rates stabilized between 2021 and 2024.
Conclusion:
AF/AFL-related heart failure mortality has increased substantially over the past 26 years in the U.S. with marked disparities by sex, race/ethnicity, region, and urbanization. While recent years have seen a plateau in mortality rates, the continued burden—especially among vulnerable populations underscores the need for equitable, targeted public health interventions and improved access to cardiovascular care.
Atrial fibrillation (AF) and heart failure (HF) are prevalent cardiovascular disorders that frequently co-occur, exacerbating each other's effects and resulting in adverse clinical outcomes. Despite the well-established association between these conditions, there is a paucity of research examining AF/atrial flutter (AFL) as direct contributors to HF-related mortality across various demographics and regions within the United States
Hypothesis:
This study aims to investigate the patterns of AF/AFL-related HF mortality in the U.S. from 1999 to 2024, stratified by age, gender, race/ethnicity, urban-rural classification, and geographic region.
Methods:
A retrospective analysis was conducted utilizing data from the Centers for Disease Control and Prevention's Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database. Mortality data were extracted from death certificates that identified AF/AFL related HF as a primary or contributing cause of death (ICD-10 codes I11.0, I13.0, I13.2, I48 and I50). Age-adjusted mortality rates (AAMRs) per 100,000 individuals were calculated, and annual percentage changes (APC) were assessed using Joinpoint regression.
Results:
From 1999 to 2024, 1,307,809 deaths in the United States were attributed to atrial fibrillation/flutter-related heart failure (AF/AFL-HF). The age-adjusted mortality rate (AAMR) rose significantly from 8.2 to 24.3 per 100,000. Males consistently had higher AAMRs than females (15.7 vs. 12.3). Racial disparities were evident, with non-Hispanic Whites having the highest cumulative AAMR (15.1), and non-Hispanic Asians/Pacific Islanders the lowest (5.7). Geographic differences were also prominent: Oregon recorded the highest state-level AAMR (25.5), while Hawaii had the lowest (8.8). Regionally, the West (15.3) and Midwest (14.9) had the highest cumulative AAMRs. Place-of-death trends showed a shift toward home deaths, which became the most common location by 2024. Although AAMRs increased sharply from 2010 to 2021 across most subgroups, rates stabilized between 2021 and 2024.
Conclusion:
AF/AFL-related heart failure mortality has increased substantially over the past 26 years in the U.S. with marked disparities by sex, race/ethnicity, region, and urbanization. While recent years have seen a plateau in mortality rates, the continued burden—especially among vulnerable populations underscores the need for equitable, targeted public health interventions and improved access to cardiovascular care.
More abstracts on this topic:
A Large Animal Model of Persistent Atrial Fibrillation
Mostafizi Pouria, Goldman Steven, Moukabary Talal, Lefkowitz Eli, Ref Jacob, Daugherty Sherry, Grijalva Adrian, Cook Kyle Eric, Chinyere Ike, Lancaster Jordan, Koevary Jen
Global, Regional, and National Trends in Atrial Fibrillation/Flutter Among Overweight and Obese Individuals: A Comparative Analysis of Gender, Age, and Risk Factors (1990-2019)Xiao Yichao, Kang Yujie, Lan Zehao, Lv Zhaohua, Liu Qiming, Zhou Shenghua