Final ID: Su4002
Effect of Combination Therapy With GLP-1 Receptor Agonists and SGLT2 Inhibitors on Cardiovascular Outcomes in Type 2 Diabetes and ASCVD: A Systematic Review and Meta-analysis
Abstract Body (Do not enter title and authors here): Background: Sodium-glucose co-transporter 2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA) have each independently demonstrated significant cardiovascular benefits in patients with type 2 diabetes mellitus (T2DM) and established atherosclerotic cardiovascular disease (ASCVD). Despite these benefits, the clinical utility of combining both therapies remains unclear.
Research question: In T2DM patients with ASCVD, does SGLT2i + GLP-1 RA therapy improve clinical outcomes versus SGLT2i alone?
Methods: We systematically searched PubMed, Embase, and Cochrane Central from inception to April 2025 for studies comparing clinical outcomes of combination therapy with SGLT2i and GLP-1 RA versus SGLT2i monotherapy in patients with T2DM and established ASCVD. For time-to-event outcomes, we pooled hazard ratios (HRs) with corresponding 95% confidence intervals (CIs), and for binary outcomes, we pooled risk ratios (RRs) with 95% CIs. All statistical analyses were performed using R software (version 4.3.1) with a random-effects model.
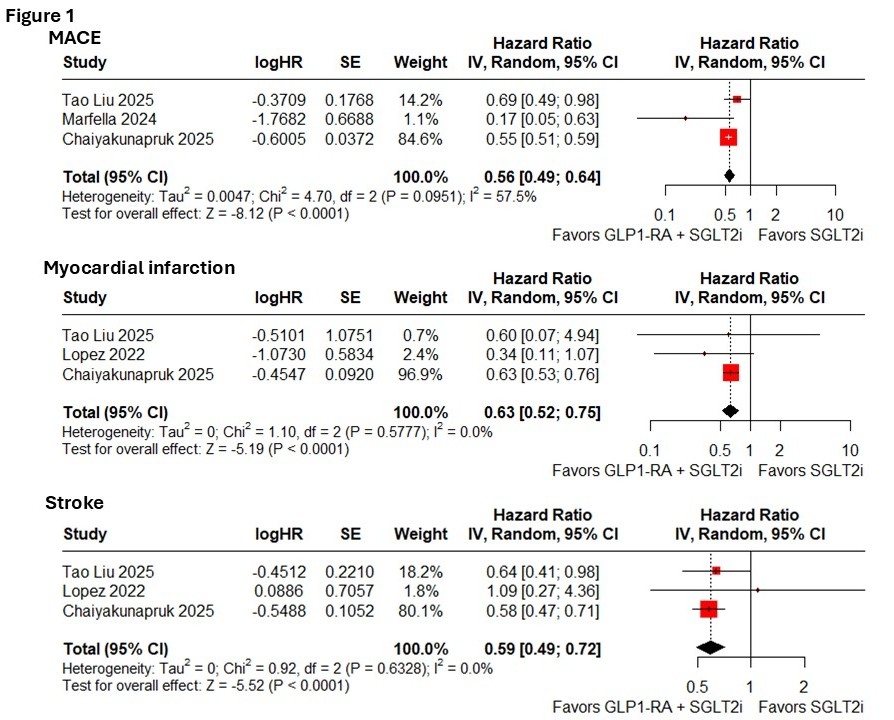
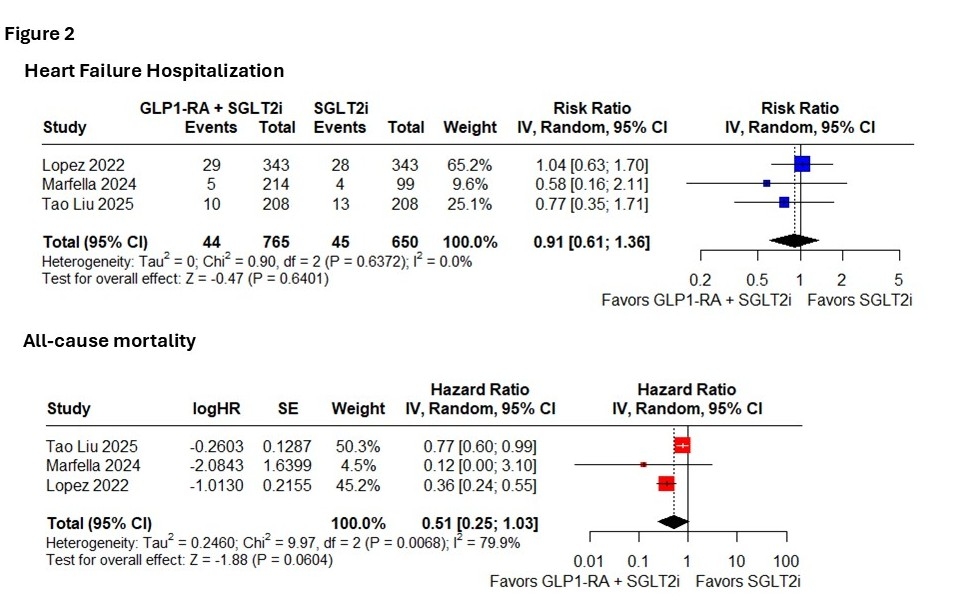
Results: Four observational studies comprising 166,325 patients were included, of whom 35,455 (21.3%) received combination therapy with a SGLT2i and a GLP-1-RA. In the pooled analysis, combination therapy was associated with a significantly lower risk of major adverse cardiovascular events (MACE) (HR 0.56 [0.49–0.64], p<0.0001), myocardial infarction (HR 0.63 [0.52–0.75], p<0.0001), and stroke (HR 0.59 [0.49–0.72], p<0.0001) compared to SGLT2i monotherapy. (Figure 1) There were no significant differences in heart failure hospitalizations (RR 0.91 [0.61–1.36], p=0.6041) or all-cause mortality (HR 0.61 [0.26–1.03], p=0.0604). (Figure 2)
Conclusion: In patients with T2DM and ASCVD, combination therapy with a GLP-1 RA and an SGLT2i was associated with significant reductions in MACE, myocardial infarction, and stroke compared to SGLT2i monotherapy. These findings suggest potential additive cardiovascular benefits from dual therapy and underscore the need for prospective trials to validate these observations.
Research question: In T2DM patients with ASCVD, does SGLT2i + GLP-1 RA therapy improve clinical outcomes versus SGLT2i alone?
Methods: We systematically searched PubMed, Embase, and Cochrane Central from inception to April 2025 for studies comparing clinical outcomes of combination therapy with SGLT2i and GLP-1 RA versus SGLT2i monotherapy in patients with T2DM and established ASCVD. For time-to-event outcomes, we pooled hazard ratios (HRs) with corresponding 95% confidence intervals (CIs), and for binary outcomes, we pooled risk ratios (RRs) with 95% CIs. All statistical analyses were performed using R software (version 4.3.1) with a random-effects model.
Results: Four observational studies comprising 166,325 patients were included, of whom 35,455 (21.3%) received combination therapy with a SGLT2i and a GLP-1-RA. In the pooled analysis, combination therapy was associated with a significantly lower risk of major adverse cardiovascular events (MACE) (HR 0.56 [0.49–0.64], p<0.0001), myocardial infarction (HR 0.63 [0.52–0.75], p<0.0001), and stroke (HR 0.59 [0.49–0.72], p<0.0001) compared to SGLT2i monotherapy. (Figure 1) There were no significant differences in heart failure hospitalizations (RR 0.91 [0.61–1.36], p=0.6041) or all-cause mortality (HR 0.61 [0.26–1.03], p=0.0604). (Figure 2)
Conclusion: In patients with T2DM and ASCVD, combination therapy with a GLP-1 RA and an SGLT2i was associated with significant reductions in MACE, myocardial infarction, and stroke compared to SGLT2i monotherapy. These findings suggest potential additive cardiovascular benefits from dual therapy and underscore the need for prospective trials to validate these observations.
More abstracts on this topic:
A multifaceted family intervention for blood pressure management in rural China: an open label, parallel group, cluster randomized trial (Healthy Family Program)
Jiang Chao, Dong Jianzeng, Cai Jun, Anderson Craig, Du Xin, Tang Yangyang, Han Rong, Song Yanna, Wang Chi, Lin Xiaolei, Yi Yang, Rodgers Anthony, Ma Changsheng
A Loss of Function Polymorphism in the Propeptide of Lysyl Oxidase Exacerbates AtherosclerosisJung In-hyuk, Amrute Junedh, Luna Sophia, Wagoner Ryan, Lee Paul, Burks Kendall, Holloway Karyn, Alisio Arturo, Stitziel Nathan