Final ID: Su3149
Double Trouble: Impact of Viral Pneumonia on Mortality and Clinical Outcomes in Patients Hospitalized with Pulmonary Embolism: A Nationwide Analysis (2016 – 2021)
Abstract Body (Do not enter title and authors here): Background
Pulmonary Embolism (PE) is a potentially life-threatening condition that warrants careful consideration of its risk factors and associated comorbidities. Viral pneumonia (VP) has been increasingly recognized as a significant risk factor for PE. The interplay between severe viral infection and coagulation abnormalities can lead to a higher incidence of thrombotic complications, multi-organ failure, and increased mortality among hospitalized patients.
Objective
To evaluate the impact of concomitant VP on outcomes in patients admitted with PE in the United States between the years 2016 - 2021.
Methods
This retrospective cohort study analyzed data from 1,120,609.4 patients hospitalized with PE without VP and 6,370.0 patients with concurrent VP. Multivariable logistic and linear regression models were utilized, adjusting for factors including age, gender, race, Charlson Comorbidity Index score, median household income, hospital region, and teaching status. The analysis focused on outcomes such as in-hospital mortality, hospital charges, complications, and length of stay.
Results
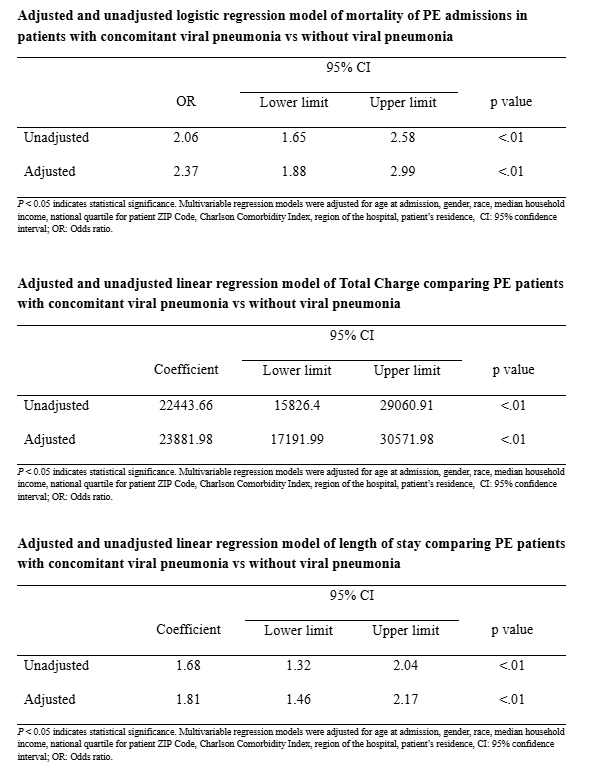
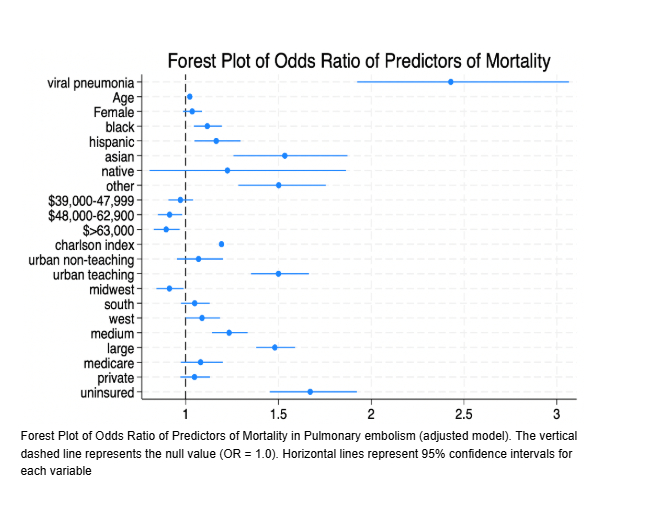
Patients hospitalized with PE and concurrent VP had significantly higher odds of in-hospital mortality compared to those without VP (Adjusted OR: 2.37; 95% CI: 1.88–2.99; P < .01). Hospital charges were also higher in the VP group—by $22,443.66 unadjusted (95% CI: $15,826.40–$29,060.91; P < .01) and $23,881.98 after OR adjustment (95% CI: $17,191.99–$30,571.98; P < .01). This may be related to a longer average hospital stay, which was 1.81 days greater in the VP group (AOR: 1.81; 95% CI: 1.46–2.17; P < .01), though not clinically significant.
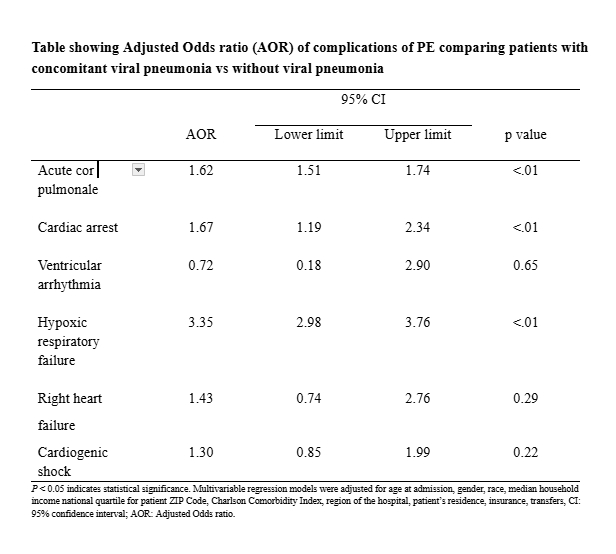
Complications were more common in PE patients with VP, including acute cor pulmonale (AOR: 1.62; 95% CI: 1.51–1.74; P < .01), cardiac arrest (AOR: 1.67; 95% CI: 1.19–2.34; P < .01), and hypoxic respiratory failure (AOR: 3.35; 95% CI: 2.98–3.76; P < .01). No significant differences were observed in the odds of ventricular arrhythmia, right heart failure, or cardiogenic shock between the two groups.
Conclusion
Patients hospitalized with PE and VP face higher risks of death, longer hospital stays, more complications, and increased healthcare costs. These findings underscore the importance of early recognition and preventive measures—like flu vaccination—to reduce the impact of viral infections on thrombotic events.
Pulmonary Embolism (PE) is a potentially life-threatening condition that warrants careful consideration of its risk factors and associated comorbidities. Viral pneumonia (VP) has been increasingly recognized as a significant risk factor for PE. The interplay between severe viral infection and coagulation abnormalities can lead to a higher incidence of thrombotic complications, multi-organ failure, and increased mortality among hospitalized patients.
Objective
To evaluate the impact of concomitant VP on outcomes in patients admitted with PE in the United States between the years 2016 - 2021.
Methods
This retrospective cohort study analyzed data from 1,120,609.4 patients hospitalized with PE without VP and 6,370.0 patients with concurrent VP. Multivariable logistic and linear regression models were utilized, adjusting for factors including age, gender, race, Charlson Comorbidity Index score, median household income, hospital region, and teaching status. The analysis focused on outcomes such as in-hospital mortality, hospital charges, complications, and length of stay.
Results
Patients hospitalized with PE and concurrent VP had significantly higher odds of in-hospital mortality compared to those without VP (Adjusted OR: 2.37; 95% CI: 1.88–2.99; P < .01). Hospital charges were also higher in the VP group—by $22,443.66 unadjusted (95% CI: $15,826.40–$29,060.91; P < .01) and $23,881.98 after OR adjustment (95% CI: $17,191.99–$30,571.98; P < .01). This may be related to a longer average hospital stay, which was 1.81 days greater in the VP group (AOR: 1.81; 95% CI: 1.46–2.17; P < .01), though not clinically significant.
Complications were more common in PE patients with VP, including acute cor pulmonale (AOR: 1.62; 95% CI: 1.51–1.74; P < .01), cardiac arrest (AOR: 1.67; 95% CI: 1.19–2.34; P < .01), and hypoxic respiratory failure (AOR: 3.35; 95% CI: 2.98–3.76; P < .01). No significant differences were observed in the odds of ventricular arrhythmia, right heart failure, or cardiogenic shock between the two groups.
Conclusion
Patients hospitalized with PE and VP face higher risks of death, longer hospital stays, more complications, and increased healthcare costs. These findings underscore the importance of early recognition and preventive measures—like flu vaccination—to reduce the impact of viral infections on thrombotic events.
More abstracts on this topic:
Minimally Adapted Influenza A Virus Provides A Model For Studying Cardiac Complications And Therapeutic Targets In Mice
Leumi Steve, Yount Jacob
A Genome-wide CRISPRi Screen Implicates Coronary Artery Disease GWAS Genes as Key Regulators of Adventitial Fibroblast ProliferationJackson William, Zhu Ashley, Gu Wenduo, Berezowitz Alexa, Iyer Meghana, Cheng Paul