Final ID: MP2257
Association of Adverse Pregnancy Outcomes with Long-Term Risk of Cardiovascular Disease and Risk Factors in a Diverse Cohort
Abstract Body (Do not enter title and authors here): Background:
Adverse pregnancy outcomes (APOs) are increasingly recognized as risk indicators for future cardiovascular disease (CVD), yet their long-term implications across diverse populations remain insufficiently understood. Current guidelines lack comprehensive strategies for post-APO CVD screening.
Objective:
To assess the association between APOs and subsequent CVD and cardiovascular risk factors (CRF) in a racially and socioeconomically diverse cohort, and to identify demographic and socioeconomic risk factors for CVD/CRF among individuals with APOs.
Methods:
This retrospective cohort study included pregnant adult members of Kaiser Permanente Northern California who delivered between July 1, 2008, and June 30, 2013, with follow-up through December 31, 2023. Patients with APOs—defined as hypertensive disorders of pregnancy, gestational diabetes, preterm delivery, placental abruption, and/or small for gestational age—were matched 1:3 by age and delivery date to those without APOs. The primary outcome was incident CVD, including coronary artery disease, acute coronary syndrome, ischemic or hemorrhagic stroke, cardiomyopathy, and atrial fibrillation/flutter. The secondary outcome was CRF, defined as incident type 2 diabetes or hypertension. Adjusted hazard ratios (aHRs) with 95% confidence intervals (CIs) were estimated.
Results:
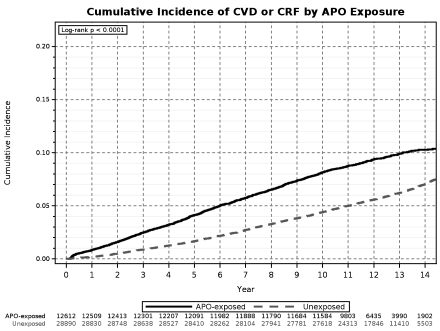
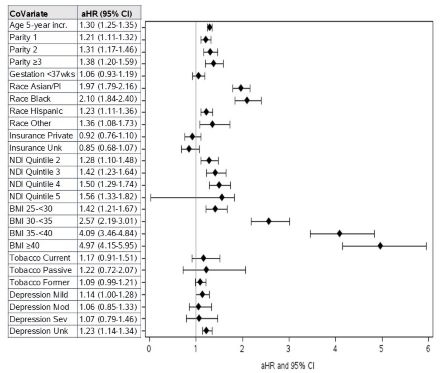
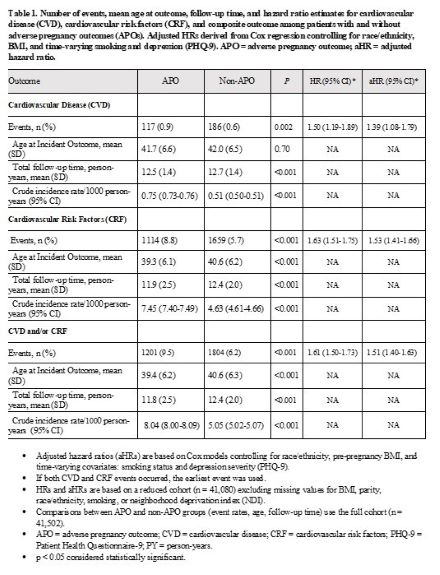
Among 41,502 participants, 12,612 (30.4%) experienced one or more APOs. Over a mean follow-up of 12.5 years, APO-exposed individuals had higher adjusted risk of CVD (aHR 1.39; 95% CI 1.08-1.79), CRF (aHR 1.53; 95% CI 1.41-1.66), and the composite outcome CVD/CRF (aHR 1.51; 95% CI 1.40-1.63). In the APO-exposed group, significant risk factors of CVD/CRF included advancing age (aHR 1.30 per 5 years; 95% CI 1.25-1.35), parity >=3 (aHR 1.38; 95% CI 1.20-1.59) vs. nulliparity, Black (aHR 2.10; 95% CI 1.84-2.40) and Asian/Pacific Islander (aHR 1.97; 95% CI 1.79-2.16) compared to White, highest neighborhood deprivation index quintile (aHR 1.56; 95% CI 1.33-1.82) vs. lowest quintile, and pre-pregnancy BMI >=40 kg/m2 (aHR 4.97; 95% CI 4.15-5.95) vs. BMI <25.
Conclusions:
APOs are associated with long-term increased risk of CVD and CRF. This risk is influenced by demographic and socioeconomic factors, emphasizing the importance of integrating reproductive history and social determinants into cardiovascular risk stratification and screening efforts.
Adverse pregnancy outcomes (APOs) are increasingly recognized as risk indicators for future cardiovascular disease (CVD), yet their long-term implications across diverse populations remain insufficiently understood. Current guidelines lack comprehensive strategies for post-APO CVD screening.
Objective:
To assess the association between APOs and subsequent CVD and cardiovascular risk factors (CRF) in a racially and socioeconomically diverse cohort, and to identify demographic and socioeconomic risk factors for CVD/CRF among individuals with APOs.
Methods:
This retrospective cohort study included pregnant adult members of Kaiser Permanente Northern California who delivered between July 1, 2008, and June 30, 2013, with follow-up through December 31, 2023. Patients with APOs—defined as hypertensive disorders of pregnancy, gestational diabetes, preterm delivery, placental abruption, and/or small for gestational age—were matched 1:3 by age and delivery date to those without APOs. The primary outcome was incident CVD, including coronary artery disease, acute coronary syndrome, ischemic or hemorrhagic stroke, cardiomyopathy, and atrial fibrillation/flutter. The secondary outcome was CRF, defined as incident type 2 diabetes or hypertension. Adjusted hazard ratios (aHRs) with 95% confidence intervals (CIs) were estimated.
Results:
Among 41,502 participants, 12,612 (30.4%) experienced one or more APOs. Over a mean follow-up of 12.5 years, APO-exposed individuals had higher adjusted risk of CVD (aHR 1.39; 95% CI 1.08-1.79), CRF (aHR 1.53; 95% CI 1.41-1.66), and the composite outcome CVD/CRF (aHR 1.51; 95% CI 1.40-1.63). In the APO-exposed group, significant risk factors of CVD/CRF included advancing age (aHR 1.30 per 5 years; 95% CI 1.25-1.35), parity >=3 (aHR 1.38; 95% CI 1.20-1.59) vs. nulliparity, Black (aHR 2.10; 95% CI 1.84-2.40) and Asian/Pacific Islander (aHR 1.97; 95% CI 1.79-2.16) compared to White, highest neighborhood deprivation index quintile (aHR 1.56; 95% CI 1.33-1.82) vs. lowest quintile, and pre-pregnancy BMI >=40 kg/m2 (aHR 4.97; 95% CI 4.15-5.95) vs. BMI <25.
Conclusions:
APOs are associated with long-term increased risk of CVD and CRF. This risk is influenced by demographic and socioeconomic factors, emphasizing the importance of integrating reproductive history and social determinants into cardiovascular risk stratification and screening efforts.
More abstracts on this topic:
A Quarter Century of Cardiovascular Risk: National Mortality Trends in Hypertension and Arrhythmias Among U.S. Adults Aged 55 and Older
Ahmad Husnain, Khan Muhammad, Sharif Aleena, Hossain Mohammad, Eltawansy Sherif, Faizan Muhammad, Ali Muhammad Faizan, Ahmed Ashraf, Abdul Malik Mohammad Hamza Bin, Pahwani Ritesh, Patel Rahul, Mehdi Hassan
Associations between Body Mass Index, Adverse Pregnancy Outcomes, and Cardiovascular Risk Factors in Midlife: A Mediation analysis in the Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) StudyBorrowman Jaclyn, Huang Xiaoning, Petito Lucia, Perak Amanda, Scholtens Denise, Lowe William, Lloyd-jones Donald, Grobman William, Khan Sadiya