Final ID: Su2123
What’s On Shelf Shapes What’s in Heart: Retail Food Environment and County-Level Cardiac Mortality in the United States, A Nationwide Ecological Study
Abstract Body (Do not enter title and authors here):
Background
Emerging evidence links the local food environment to chronic disease outcomes, yet its relationship with cardiac mortality remains under explored at the population level. This study examines the association between the Retail Food Environment Index (RFEI), a marker of community food healthiness, and cardiac death rates across U.S. counties.
Hypothesis
We propose that higher RFEI scores are significantly linked to greater cardiac mortality, independent of socioeconomic status, lifestyle behaviours, and demographic characteristics.
Methods
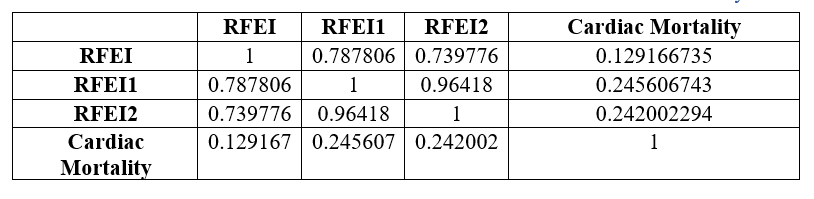
A cross-sectional ecological study was conducted using county-level data from 2,793 U.S. counties, integrating cardiac mortality information from the CDC WONDER database for the years 2018–2020 and the food accessibility data from the USDA Food Environment Atlas. The primary outcome was age-adjusted cardiac mortality per 100,000 population. The main exposure variable was the Retail Food Environment Index (RFEI), defined as the ratio of fast-food outlets and convenience stores to supermarkets and farmers' markets. To test the robustness of the RFEI, two alternate indices (RFEI1 and RFEI2) were developed by varying the inclusion criteria for superstore classification.
Descriptive statistics, along with univariable and multivariable regression analyses, were performed, adjusting for socioeconomic indicators, racial/ethnic composition, health behaviours, metabolic risk factors, and food accessibility.
Results
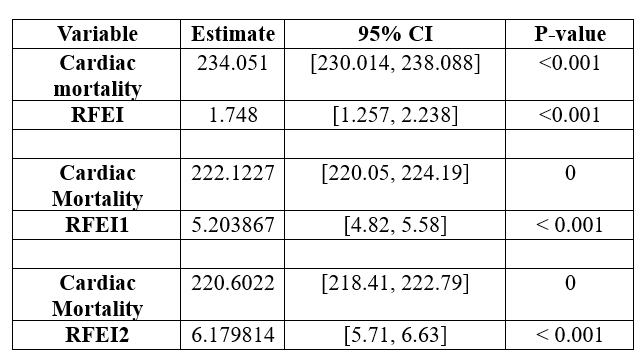
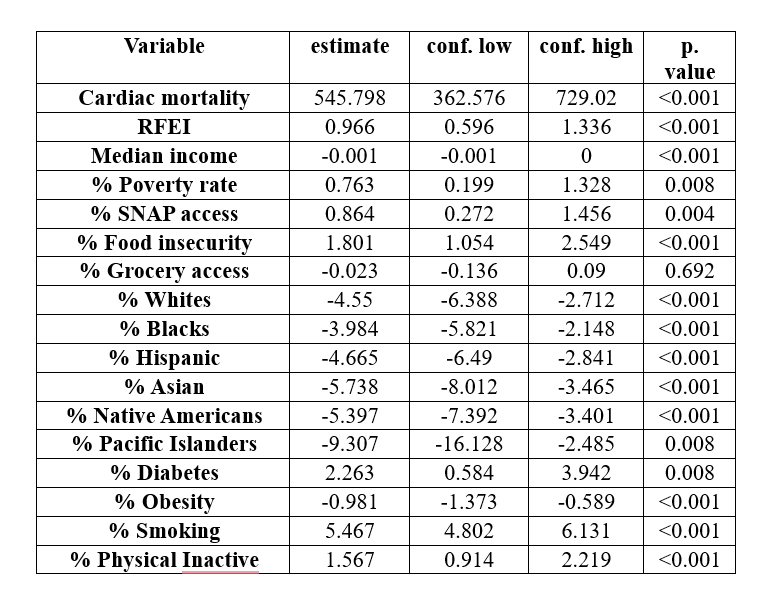
The mean cardiac mortality rate was 246.6 per 100,000 (SD = 58.3). RFEI showed a positive association with cardiac mortality in both univariate (β = 1.75; 95% CI, 1.25–2.24; P < 0.001) and multivariable analyses (β = 0.96; 95% CI, 0.60–1.34; P < 0.001). RFEI1 and RFEI2 yielded consistent results (β = 2.17 and 2.37, respectively; both P < 0.001). Among covariates, smoking (β = 5.47; P < 0.001), diabetes (β = 2.26; P = 0.008), and poverty rate (β = 0.76; P = 0.008) were significant predictors. The final model explained 50% of the variation in mortality (adjusted R square = 0.50).
Conclusion
A higher density of unhealthy food outlets is independently associated with increased cardiac mortality across U.S. counties. These findings underscore the importance of local food environments as modifiable population-level determinants of cardiovascular health and support public health strategies aimed at improving equitable access to nutritious food.
Background
Emerging evidence links the local food environment to chronic disease outcomes, yet its relationship with cardiac mortality remains under explored at the population level. This study examines the association between the Retail Food Environment Index (RFEI), a marker of community food healthiness, and cardiac death rates across U.S. counties.
Hypothesis
We propose that higher RFEI scores are significantly linked to greater cardiac mortality, independent of socioeconomic status, lifestyle behaviours, and demographic characteristics.
Methods
A cross-sectional ecological study was conducted using county-level data from 2,793 U.S. counties, integrating cardiac mortality information from the CDC WONDER database for the years 2018–2020 and the food accessibility data from the USDA Food Environment Atlas. The primary outcome was age-adjusted cardiac mortality per 100,000 population. The main exposure variable was the Retail Food Environment Index (RFEI), defined as the ratio of fast-food outlets and convenience stores to supermarkets and farmers' markets. To test the robustness of the RFEI, two alternate indices (RFEI1 and RFEI2) were developed by varying the inclusion criteria for superstore classification.
Descriptive statistics, along with univariable and multivariable regression analyses, were performed, adjusting for socioeconomic indicators, racial/ethnic composition, health behaviours, metabolic risk factors, and food accessibility.
Results
The mean cardiac mortality rate was 246.6 per 100,000 (SD = 58.3). RFEI showed a positive association with cardiac mortality in both univariate (β = 1.75; 95% CI, 1.25–2.24; P < 0.001) and multivariable analyses (β = 0.96; 95% CI, 0.60–1.34; P < 0.001). RFEI1 and RFEI2 yielded consistent results (β = 2.17 and 2.37, respectively; both P < 0.001). Among covariates, smoking (β = 5.47; P < 0.001), diabetes (β = 2.26; P = 0.008), and poverty rate (β = 0.76; P = 0.008) were significant predictors. The final model explained 50% of the variation in mortality (adjusted R square = 0.50).
Conclusion
A higher density of unhealthy food outlets is independently associated with increased cardiac mortality across U.S. counties. These findings underscore the importance of local food environments as modifiable population-level determinants of cardiovascular health and support public health strategies aimed at improving equitable access to nutritious food.
More abstracts on this topic:
Adherence to Dutch dietary guidelines and long-term mortality risk in post-myocardial infarction patients of the Alpha Omega Cohort
Cruijsen Esther, Van Damme Iris, Visseren Frank, Geleijnse Johanna
Acute Exposure to High PM2.5 Levels Increases the Risk of Late All-Cause Mortality in Patients with STEMIFathieh Sina, Tran Hao, Faour Amir, Pahn Reece, Long Mitchell, Tam Gladys, Figtree Gemma, Negishi Kazuaki, French John