Final ID: Su2060
Re-evaluating the Reliability of Size as a Biomarker for Monitoring Paraganglioma Activity
Abstract Body (Do not enter title and authors here): Case Description:
A 38-year-old woman with a history of hypertension presented in 2016 with right-sided abdominal pain. Imaging revealed a 1.7 x 2.3 cm left periaortic mass near the diaphragmatic hiatus. The mass was considered likely benign and asymptomatic, with surveillance MRIs showing stability over 9 months.
In 2018, she developed episodic chest pain, headaches, and hypertension. Workup for secondary hypertension showed mildly elevated catecholamine levels, but results were deemed clinically insignificant.
From 2018 to 2021, annual MRIs showed the patient’s mass remained stable. However, in 2024, the patient experienced worsening hypertensive episodes with headaches, palpitations, chest pain, and a 15-pound weight loss. Her symptoms persisted despite anti-hypertensives.
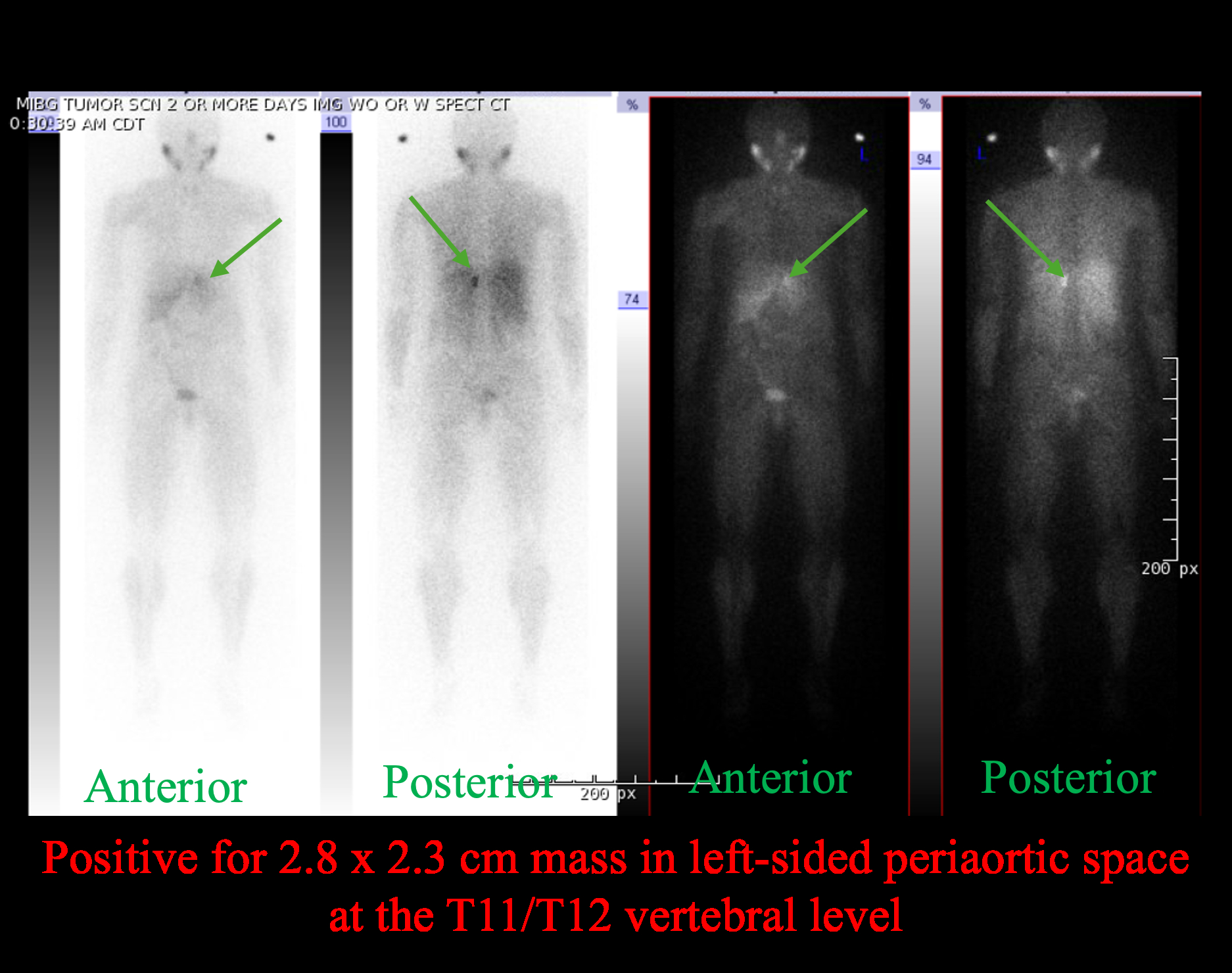
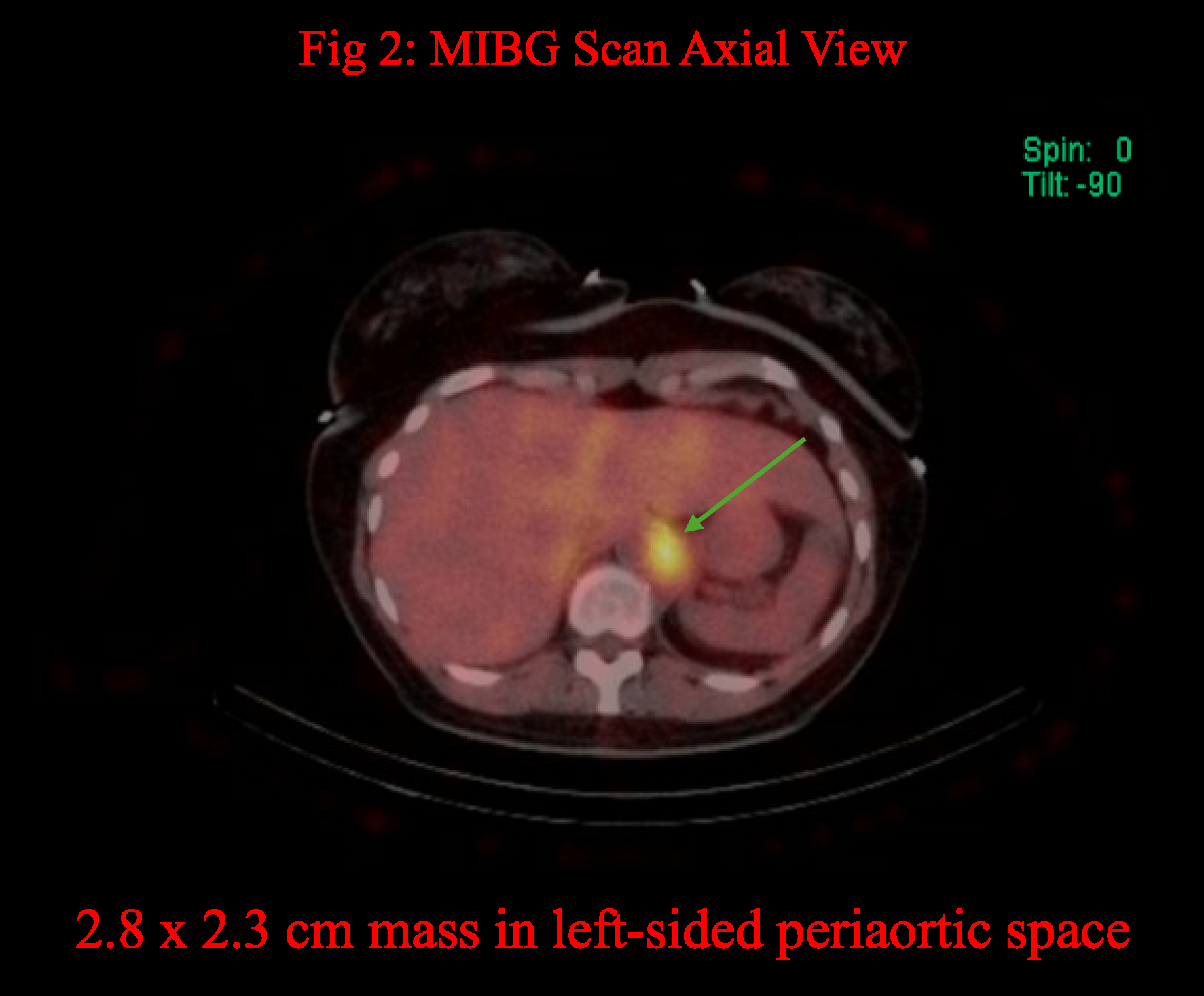
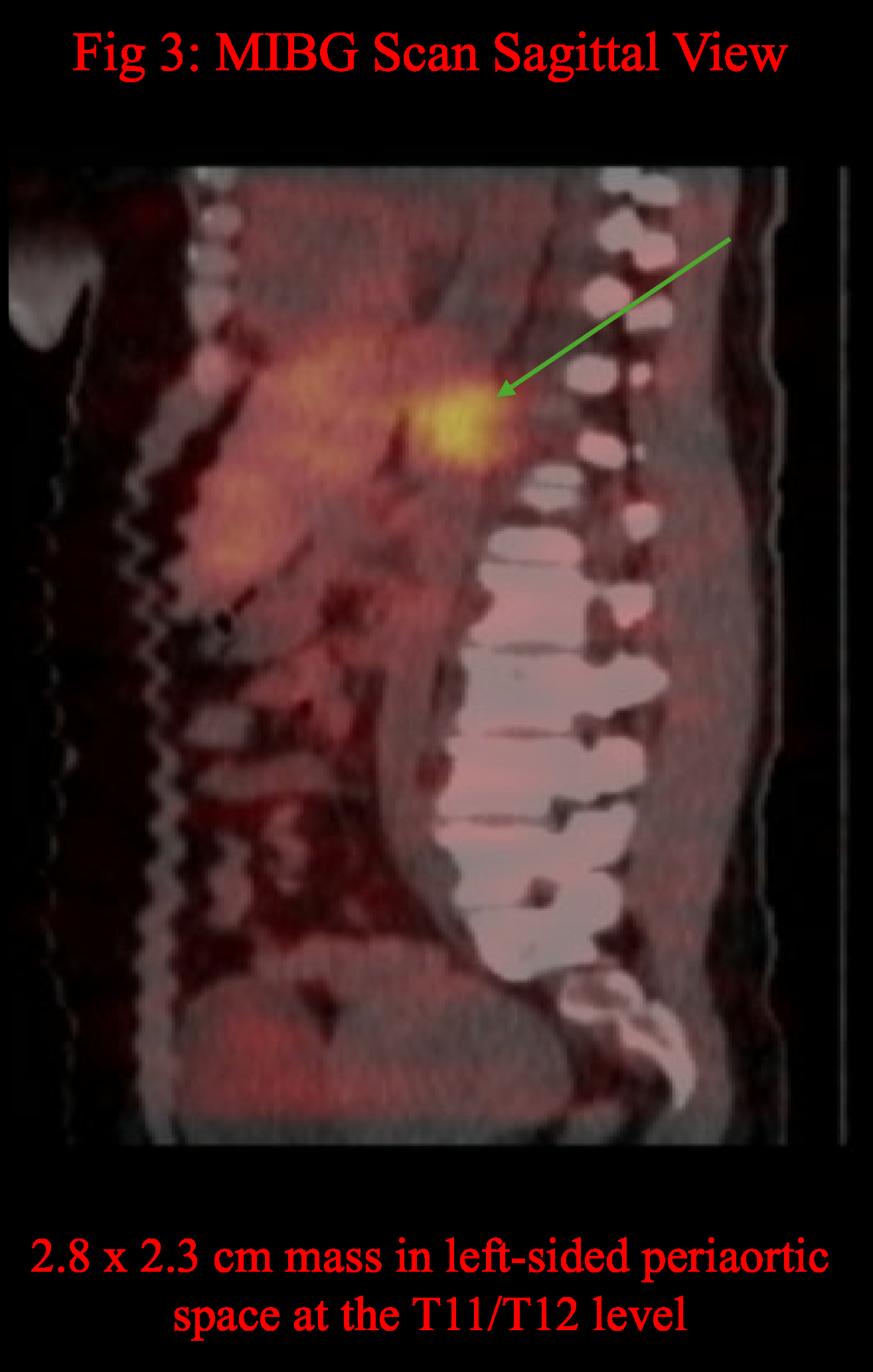
At the Rush Heart Center for Women, testing showed significantly elevated plasma and 24-hour urine normetanephrine levels. An MIBG scan with CT/SPECT identified a 2.8 × 2.3 cm mass near T11/T12, likely paraganglioma.
In January 2025, the mass was resected, and the patient has since reported significant symptom improvement.
Discussion:
The patient experienced episodic blood pressure spikes beginning in 2013. A periaortic mass was noted on CT in 2016, and mildly elevated metanephrines were documented in 2018, but her symptoms continued to be managed as essential hypertension. Over the next several years, despite worsening hypertensive crises, her workup was not pursued further. A catecholamine-secreting lesion was finally diagnosed in 2024 followed by resection in January 2025. This eight-year diagnostic delay severely affected her quality of life and underscores the need for a broad differential for hypertension among cardiologists—particularly considering rare causes like paraganglioma—when patients have persistent, treatment-refractory hypertension.
Current research links larger paragangliomas (>4 cm) with more symptoms, higher metanephrine levels, and increased metastatic risk, showing a correlation between tumor size and normetanephrine levels. However, in this patient, the tumor size remained stable on imaging while symptoms worsened, suggesting increasing metabolic activity. This case questions the reliability of tumor size as a marker of metabolic activity and highlights the possibility that slow-growing paragangliomas may become metabolically active before changes are visible on imaging. Further research is necessary to better understand this relationship and enhance patient care.
A 38-year-old woman with a history of hypertension presented in 2016 with right-sided abdominal pain. Imaging revealed a 1.7 x 2.3 cm left periaortic mass near the diaphragmatic hiatus. The mass was considered likely benign and asymptomatic, with surveillance MRIs showing stability over 9 months.
In 2018, she developed episodic chest pain, headaches, and hypertension. Workup for secondary hypertension showed mildly elevated catecholamine levels, but results were deemed clinically insignificant.
From 2018 to 2021, annual MRIs showed the patient’s mass remained stable. However, in 2024, the patient experienced worsening hypertensive episodes with headaches, palpitations, chest pain, and a 15-pound weight loss. Her symptoms persisted despite anti-hypertensives.
At the Rush Heart Center for Women, testing showed significantly elevated plasma and 24-hour urine normetanephrine levels. An MIBG scan with CT/SPECT identified a 2.8 × 2.3 cm mass near T11/T12, likely paraganglioma.
In January 2025, the mass was resected, and the patient has since reported significant symptom improvement.
Discussion:
The patient experienced episodic blood pressure spikes beginning in 2013. A periaortic mass was noted on CT in 2016, and mildly elevated metanephrines were documented in 2018, but her symptoms continued to be managed as essential hypertension. Over the next several years, despite worsening hypertensive crises, her workup was not pursued further. A catecholamine-secreting lesion was finally diagnosed in 2024 followed by resection in January 2025. This eight-year diagnostic delay severely affected her quality of life and underscores the need for a broad differential for hypertension among cardiologists—particularly considering rare causes like paraganglioma—when patients have persistent, treatment-refractory hypertension.
Current research links larger paragangliomas (>4 cm) with more symptoms, higher metanephrine levels, and increased metastatic risk, showing a correlation between tumor size and normetanephrine levels. However, in this patient, the tumor size remained stable on imaging while symptoms worsened, suggesting increasing metabolic activity. This case questions the reliability of tumor size as a marker of metabolic activity and highlights the possibility that slow-growing paragangliomas may become metabolically active before changes are visible on imaging. Further research is necessary to better understand this relationship and enhance patient care.
More abstracts on this topic:
A Growing Burden of Electronic Medical Record Messages in ACHD Care
Dailey Schwartz Andrew, Alegria Jorge
10-Year Trend Analysis of Medicare Payment in Stroke Inpatient Hospital AdmissionWong Ka-ho, Krothapalli Neeharika, Littig Lauren, Champagne Alison, Majersik Jennifer, Reddy Vivek, De Havenon Adam