Final ID: MP1713
Metabolic Health, Arterial Stiffness, and Incident Cardiovascular Diseases: The Framingham Heart Study
Abstract Body (Do not enter title and authors here): BACKGROUND: It has been established that metabolic syndrome (MetS), its subclinical counterpart (insulin resistance, IR), and arterial stiffness (AS) are prominent markers of cardiovascular risk; however, the magnitude of their joint association is not well established.
OBJECTIVE: To investigate the potential impact of the joint association of metabolic syndrome and insulin resistance with arterial stiffness on the risk of incident cardiovascular diseases.
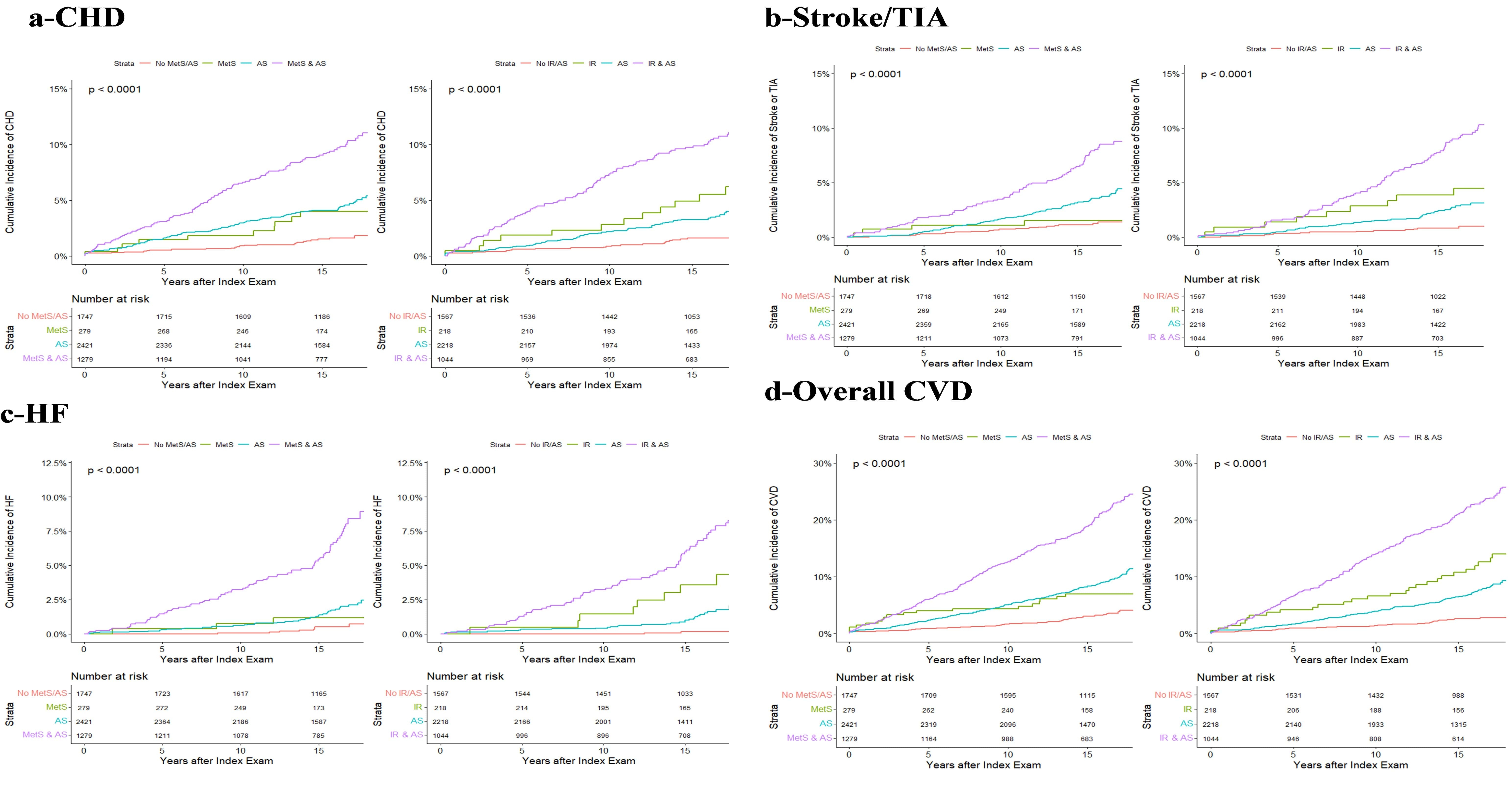
METHODS: AS was defined by carotid-femoral pulse wave velocity, augmentation index, central pulse pressure, carotid-brachial pulse wave velocity, carotid-radial pulse wave velocity, or brachial pulse pressure ≥ 75th percentile. Participants were classified in four categories based on the presence or absence of MetS/IR and AS, with the group without any of these disorders considered as reference. Outcomes included incident coronary heart disease (CHD), stroke or transient ischemic attack (TIA), heart failure (HF), overall CVD (composite of CHD, stroke/TIA, and HF, whichever occurred first), and mortality (all-cause and cardiovascular). Cox proportional hazards models were used.
RESULTS: RESULTS: 5,726 subjects (45.6% men, 4.8% with diabetes, mean age 46.86 years) were included. Over a median of 16.65 years, 271 participants (4.7%) developed CHD, 199 stroke/TIA (3.5%), 144 HF (2.5%), 562 (9.8%) overall CVD, and 641 died (11.2%). After adjustment for confounders, compared to participants with no AS and no MetS, those with AS only were at higher risk of CHD (HR 1.58, 95% CI 1.03 - 2.45), those with MetS only had no significant difference in the risk of all outcomes, and those with AS and MetS were at higher risk of CHD (HR 2.12, 95% CI 1.35 - 3.33), stroke/TIA (HR 1.72, 95% CI 1.02 - 2.92), overall CVD (HR 2.01, 95% CI 1.47 - 2.75), and cardiovascular death (HR 2.75, 95% CI 1.07 - 7.06). In participants without diabetes, compared to subjects with no AS and no IR, those with AS only were at higher risk of overall CVD (HR 1.47, 95% CI 1.02 - 2.12), those with MetS only were at higher risk of HF (HR 6.42, 95% CI 1.29 - 31.80) and overall CVD (HR 1.89, 95% CI 1.11 - 3.22), and those with AS and MetS were at higher risk of CHD (HR 2.01, 95% CI 1.17 - 3.42), stroke/TIA (HR 2.54, 95% CI 1.28 - 5.04), HF (HR 5.91, 95% CI 1.36 - 25.74), and overall CVD (HR 2.25, 95% CI 1.50 - 3.36).
CONCLUSION: In a large community-based population, the joint association of MetS or IR with AS predisposed to increased risks of CVD.
OBJECTIVE: To investigate the potential impact of the joint association of metabolic syndrome and insulin resistance with arterial stiffness on the risk of incident cardiovascular diseases.
METHODS: AS was defined by carotid-femoral pulse wave velocity, augmentation index, central pulse pressure, carotid-brachial pulse wave velocity, carotid-radial pulse wave velocity, or brachial pulse pressure ≥ 75th percentile. Participants were classified in four categories based on the presence or absence of MetS/IR and AS, with the group without any of these disorders considered as reference. Outcomes included incident coronary heart disease (CHD), stroke or transient ischemic attack (TIA), heart failure (HF), overall CVD (composite of CHD, stroke/TIA, and HF, whichever occurred first), and mortality (all-cause and cardiovascular). Cox proportional hazards models were used.
RESULTS: RESULTS: 5,726 subjects (45.6% men, 4.8% with diabetes, mean age 46.86 years) were included. Over a median of 16.65 years, 271 participants (4.7%) developed CHD, 199 stroke/TIA (3.5%), 144 HF (2.5%), 562 (9.8%) overall CVD, and 641 died (11.2%). After adjustment for confounders, compared to participants with no AS and no MetS, those with AS only were at higher risk of CHD (HR 1.58, 95% CI 1.03 - 2.45), those with MetS only had no significant difference in the risk of all outcomes, and those with AS and MetS were at higher risk of CHD (HR 2.12, 95% CI 1.35 - 3.33), stroke/TIA (HR 1.72, 95% CI 1.02 - 2.92), overall CVD (HR 2.01, 95% CI 1.47 - 2.75), and cardiovascular death (HR 2.75, 95% CI 1.07 - 7.06). In participants without diabetes, compared to subjects with no AS and no IR, those with AS only were at higher risk of overall CVD (HR 1.47, 95% CI 1.02 - 2.12), those with MetS only were at higher risk of HF (HR 6.42, 95% CI 1.29 - 31.80) and overall CVD (HR 1.89, 95% CI 1.11 - 3.22), and those with AS and MetS were at higher risk of CHD (HR 2.01, 95% CI 1.17 - 3.42), stroke/TIA (HR 2.54, 95% CI 1.28 - 5.04), HF (HR 5.91, 95% CI 1.36 - 25.74), and overall CVD (HR 2.25, 95% CI 1.50 - 3.36).
CONCLUSION: In a large community-based population, the joint association of MetS or IR with AS predisposed to increased risks of CVD.
More abstracts on this topic:
Association of Cardiovascular-Kidney-Metabolic Syndrome Severity with Low Bone Mineral Density: NHANES 2005-2018
Agordekpe Ethel, Echouffo Justin, Fang Michael
Cardiac Branched-Chain Amino Acid Metabolic Dysfunction in a Novel Model of Diabetic CardiomyopathyNagao Manabu, Asakura Junko, Hosooka Tetsuya, Kuwahara Naoya, Kaneshiro Kenta, Tanaka Hidekazu, Ishida Tatsuro, Otake Hiromasa, Shinohara Masakazu