Final ID: MP233
Healthcare-related social determinants of health are associated with pain severity among adults with comorbid heart failure and chronic pain
Abstract Body (Do not enter title and authors here): Introduction: Chronic pain worsens symptom burden, physical function, and quality of life in heart failure (HF). Social determinants of health (SDOH) can shape the trajectory of HF and other disease states. Healthcare-related SDOH may also be related to the severity of pain among people with HF, but these relationships are unexplored. The aims among adults with HF and chronic pain were to: 1) describe healthcare-related SDOH; 2) compare healthcare utilization by pain severity; and 3) examine the relationship between healthcare-related SDOH and pain severity.
Methods: In this cross-sectional study, descriptive statistics and multiple linear regression were used to analyze data from 3,988 participants with HF and chronic pain enrolled in the All of Us Research Program. Pain severity was assessed using a 0-10 scale. Healthcare-related SDOH variables were insurance coverage, self-reported access barriers, and healthcare affordability. Healthcare utilization variables were the number of general provider visits, prescribing advanced practice clinician visits, and specialist visits in the past 12 months.
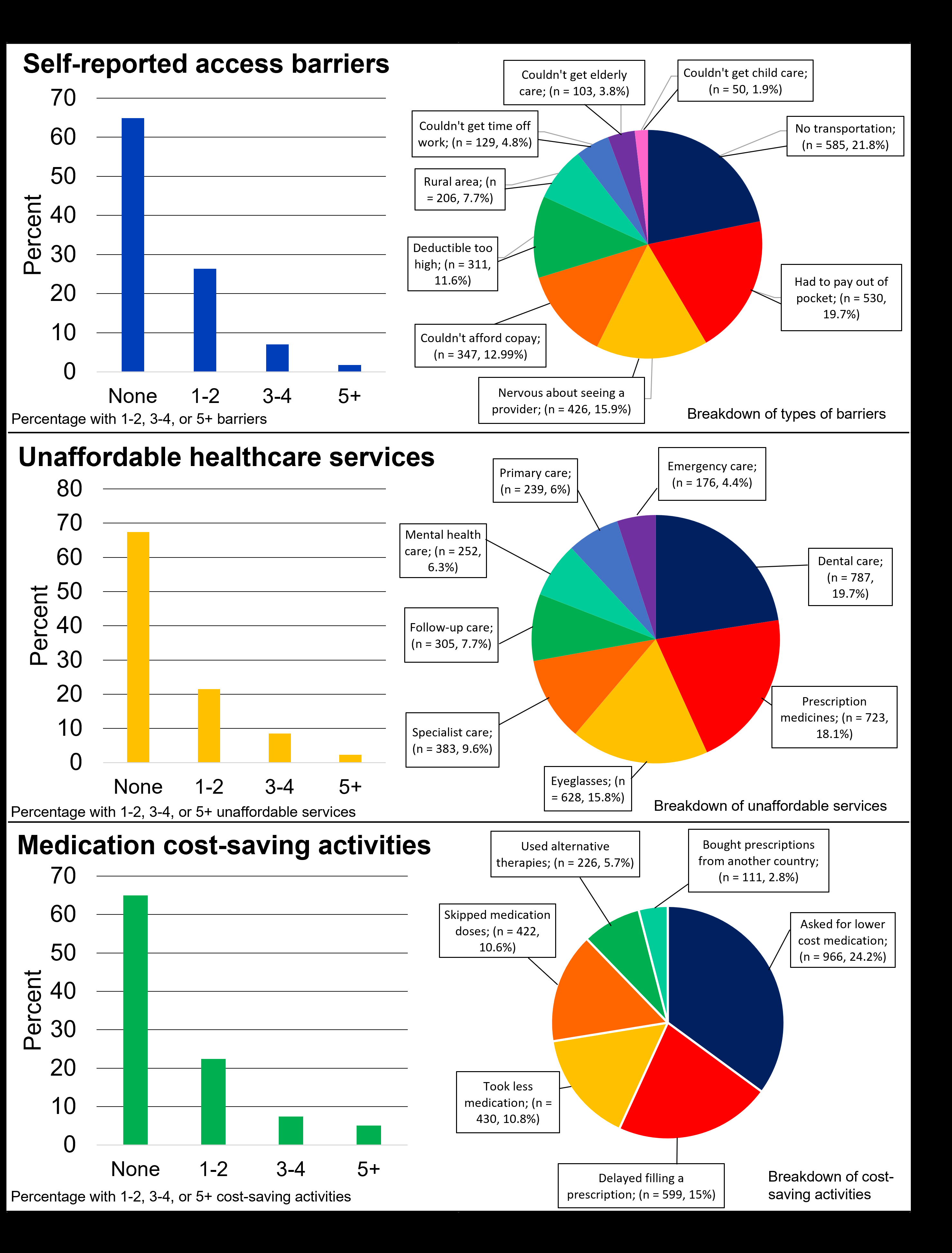
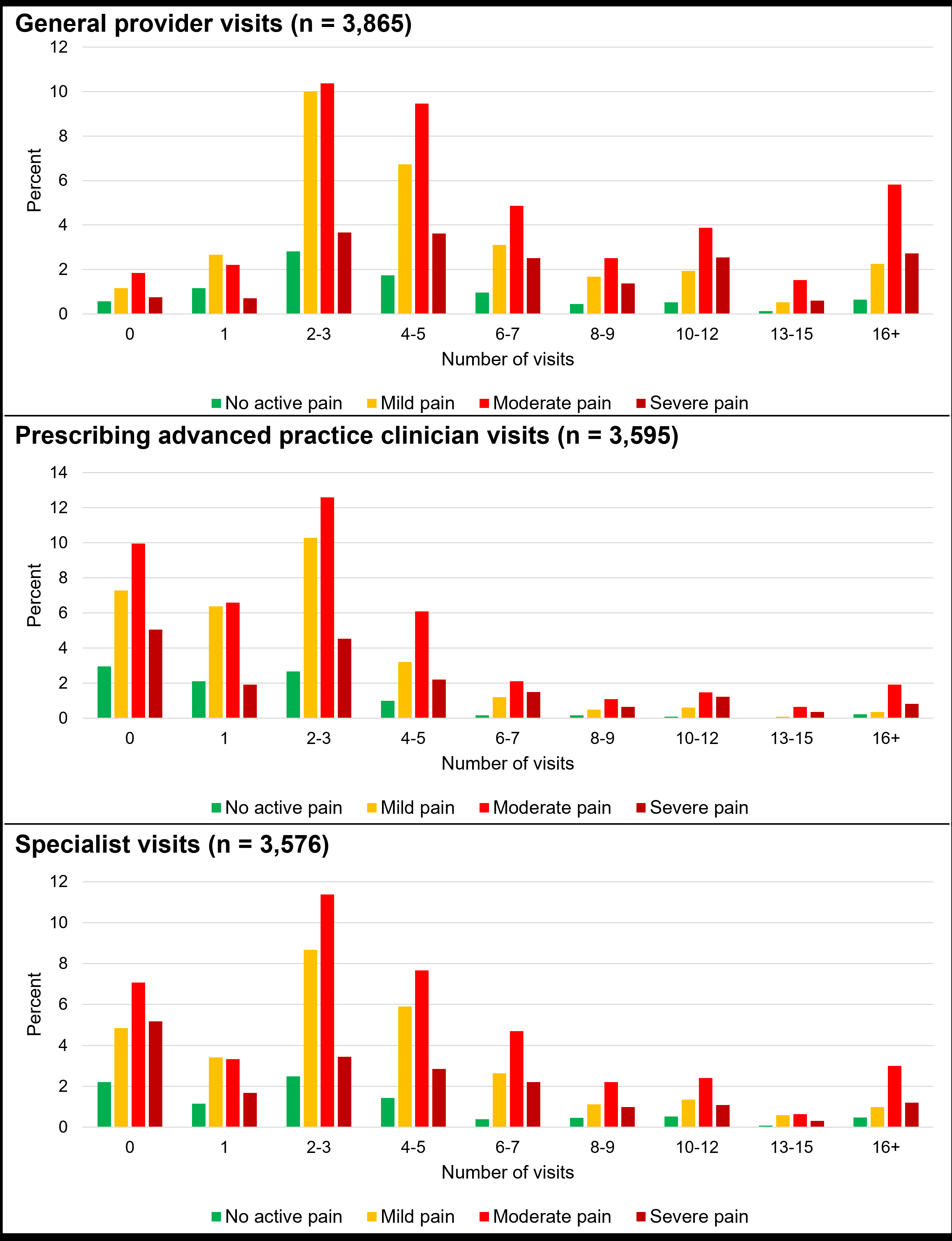
Results: The sample was mean age 70.04 years, 58% female, and 69.8% White race. Over 98% of participants had health insurance. The most common self-reported access barrier, unaffordable service, and medication cost-saving behavior was “no transportation” (14.7%), “dental care” (19.7%), and “asking for lower cost prescriptions” (24.2%), respectively (see Figure 1). Most participants saw a provider 2-3 times over 12 months, but those with higher pain severity saw a general provider more frequently than other pain groups (see Figure 2).
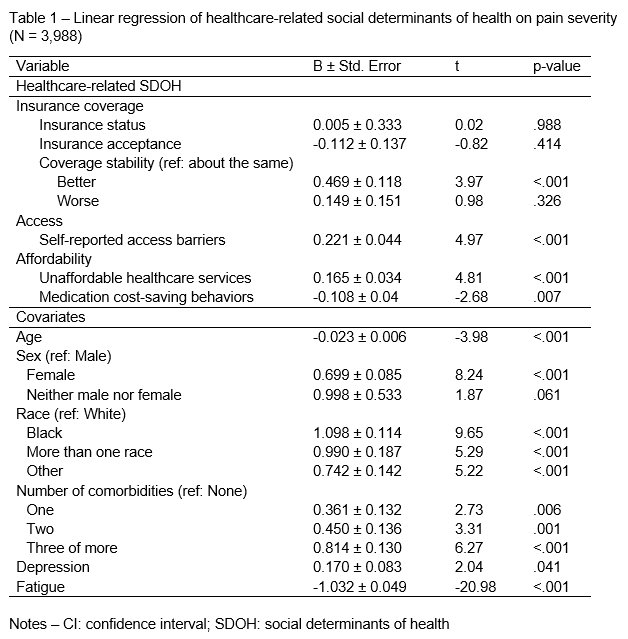
Participants with a higher number of self-reported access barriers (β = 0.221 ± 0.044, p < .001), and a higher number of unaffordable services (β = 0.165 ± 0.034, p < .001), experienced higher pain severity. In contrast, participants who adopted a higher number of medication cost-saving behaviors experienced significantly lower pain severity (β = -0.108 ± 0.040, p = .007). Participants who were younger, female sex, non-White race, had more comorbidities, a positive depression diagnosis, and lower reported fatigue, experienced significantly higher pain severity (see Table 1).
Conclusions: Despite the high percentage of insured participants, there were notable access and affordability barriers, which were associated with pain severity. These barriers should be confirmed with targeted studies that directly examine pain-related services.
Methods: In this cross-sectional study, descriptive statistics and multiple linear regression were used to analyze data from 3,988 participants with HF and chronic pain enrolled in the All of Us Research Program. Pain severity was assessed using a 0-10 scale. Healthcare-related SDOH variables were insurance coverage, self-reported access barriers, and healthcare affordability. Healthcare utilization variables were the number of general provider visits, prescribing advanced practice clinician visits, and specialist visits in the past 12 months.
Results: The sample was mean age 70.04 years, 58% female, and 69.8% White race. Over 98% of participants had health insurance. The most common self-reported access barrier, unaffordable service, and medication cost-saving behavior was “no transportation” (14.7%), “dental care” (19.7%), and “asking for lower cost prescriptions” (24.2%), respectively (see Figure 1). Most participants saw a provider 2-3 times over 12 months, but those with higher pain severity saw a general provider more frequently than other pain groups (see Figure 2).
Participants with a higher number of self-reported access barriers (β = 0.221 ± 0.044, p < .001), and a higher number of unaffordable services (β = 0.165 ± 0.034, p < .001), experienced higher pain severity. In contrast, participants who adopted a higher number of medication cost-saving behaviors experienced significantly lower pain severity (β = -0.108 ± 0.040, p = .007). Participants who were younger, female sex, non-White race, had more comorbidities, a positive depression diagnosis, and lower reported fatigue, experienced significantly higher pain severity (see Table 1).
Conclusions: Despite the high percentage of insured participants, there were notable access and affordability barriers, which were associated with pain severity. These barriers should be confirmed with targeted studies that directly examine pain-related services.
More abstracts on this topic:
A Comparison of Anxiety and Depression in Patients with Symptoms of Palpitations Compared to High Risk Arrythmia Patients.
Treuth Mark, Patel Kunnal, Rissmiller Justin, Holdai Veera
4-Hydroxy-2-Nonenal Alters Alternative Polyadenylation to Regulate mRNA Isoform Diversity in the Transition from Human Cardiac Fibroblasts to MyofibroblastsNatarajan Kartiga, Neupane Rahul, Yalamanchili Hari Krishna, Palaniyandi Suresh, Wagner Eric, Guha Ashrith, Amirthalingam Thandavarayan Rajarajan