Final ID: Su2013
Machine Learning–Derived Patient Subgroups in Inpatient Cardiac Arrest: A National Inpatient Sample Analysis
Abstract Body (Do not enter title and authors here): Background:
In-hospital cardiac arrest (IHCA) affects over 60,000 patients annually in the U.S., yet presentations and outcomes are highly heterogeneous. Unsupervised phenotyping using administrative claims may uncover latent subgroups with distinct clinical trajectories, guiding targeted postarrest strategies.
Methods:
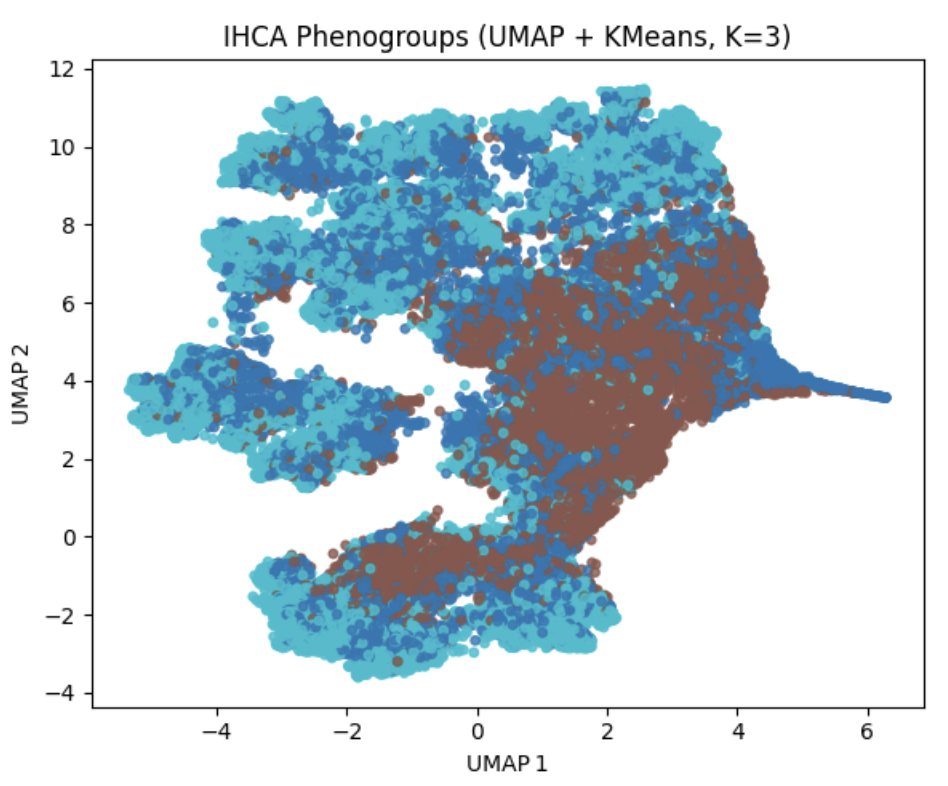
We conducted a retrospective cohort study of adult IHCA admissions from the 2021–2022 National Inpatient Sample. We identified 66,899 cases and selected multiple variables for clustering: demographics (age, sex, race, ZIP-income, payer), hospital factors (teaching status, region, bed size), Elixhauser comorbidity burden, key procedures (PCI, IABP, Impella, VA-ECMO, ventilation), and complications (sepsis, pneumonia, stroke, new atrial fibrillation, PE). After imputation, one-hot encoding, and UMAP dimensionality reduction, K-means identified three clusters. Mortality associations were assessed via multivariable logistic regression.
Results:
Three phenogroups emerged: (1) Younger, PCI-intensive (n=20,391): mean age 46 y, highest PCI (5.5%), lowest sepsis (33.3%), mortality 60.9%; (2) Middle-aged, sepsis-predominant (n=21,523): mean age 67 y, longest LOS (15.7 d), highest sepsis (47.3%), lowest PCI (2.8%), mortality 60.3%; (3) Elderly, rapidly fatal (n=24,985): mean age 76 y, shortest LOS (5.3 d), highest mortality (73.8%). Adjusted Rand Index = 0.49. Compared to cluster 2 (reference), cluster 1 had higher odds of mortality (OR 1.97; 95% CI 1.84–2.11), and cluster 3 had higher odds (OR 2.40; 95% CI 2.26–2.54; p<0.001). Independent predictors of higher mortality included female sex (OR 1.17), Black (OR 1.07) and Hispanic race (OR 1.28), older age (per year: OR 1.02), and higher Elixhauser score (per point: OR 1.16; all p<0.005).
Conclusion:
Unsupervised clustering revealed three reproducible, clinically distinct IHCA phenotypes with different mortality risks not fully captured by traditional covariates. Integrating phenogroup membership into postarrest care may enhance precision management—optimizing revascularization, sepsis protocols, and goals-of-care alignment—ultimately improving IHCA outcomes.
In-hospital cardiac arrest (IHCA) affects over 60,000 patients annually in the U.S., yet presentations and outcomes are highly heterogeneous. Unsupervised phenotyping using administrative claims may uncover latent subgroups with distinct clinical trajectories, guiding targeted postarrest strategies.
Methods:
We conducted a retrospective cohort study of adult IHCA admissions from the 2021–2022 National Inpatient Sample. We identified 66,899 cases and selected multiple variables for clustering: demographics (age, sex, race, ZIP-income, payer), hospital factors (teaching status, region, bed size), Elixhauser comorbidity burden, key procedures (PCI, IABP, Impella, VA-ECMO, ventilation), and complications (sepsis, pneumonia, stroke, new atrial fibrillation, PE). After imputation, one-hot encoding, and UMAP dimensionality reduction, K-means identified three clusters. Mortality associations were assessed via multivariable logistic regression.
Results:
Three phenogroups emerged: (1) Younger, PCI-intensive (n=20,391): mean age 46 y, highest PCI (5.5%), lowest sepsis (33.3%), mortality 60.9%; (2) Middle-aged, sepsis-predominant (n=21,523): mean age 67 y, longest LOS (15.7 d), highest sepsis (47.3%), lowest PCI (2.8%), mortality 60.3%; (3) Elderly, rapidly fatal (n=24,985): mean age 76 y, shortest LOS (5.3 d), highest mortality (73.8%). Adjusted Rand Index = 0.49. Compared to cluster 2 (reference), cluster 1 had higher odds of mortality (OR 1.97; 95% CI 1.84–2.11), and cluster 3 had higher odds (OR 2.40; 95% CI 2.26–2.54; p<0.001). Independent predictors of higher mortality included female sex (OR 1.17), Black (OR 1.07) and Hispanic race (OR 1.28), older age (per year: OR 1.02), and higher Elixhauser score (per point: OR 1.16; all p<0.005).
Conclusion:
Unsupervised clustering revealed three reproducible, clinically distinct IHCA phenotypes with different mortality risks not fully captured by traditional covariates. Integrating phenogroup membership into postarrest care may enhance precision management—optimizing revascularization, sepsis protocols, and goals-of-care alignment—ultimately improving IHCA outcomes.
More abstracts on this topic:
A Multi-Tier, Natural-Language Processing Framework to Automate Labeling of Acute Cerebrovascular Events From Radiology Reports and Diagnosis Codes
Erekat Asala, Stein Laura, Delman Bradley, Karp Adam, Kupersmith Mark, Kummer Benjamin
A Rare Case of Adalimumab-Induced Cardiac Tamponade in a Patient with Psoriatic ArthritisRaval Akhinav, Tran Minh, Saini Ishveen, Rea Mark