Final ID: MP52
Massive Aortic Root Thrombus and Coronary Embolization in a Heart Transplant Recipient on Venoarterial Extracorporeal Membrane Oxygenation (VA-ECMO) for Graft Dysfunction: An Imaging Case Report
Abstract Body (Do not enter title and authors here): A 44-year-old recent heart transplant recipient supported by VA-ECMO presented to the operating room (OR) for left ventricular (LV) vent removal. She had a history of double-inlet LV with right atrioventricular valve atresia and transposition of great arteries, status post fenestrated Fontan complicated by end-stage heart failure. Three days ago, she underwent a fourth sternotomy and orthotopic heart transplant complicated by coagulopathy and severe bi-ventricular dysfunction necessitating initiation of central VA-ECMO. Due to massive blood product transfusion and ventricular dilatation, an apical LV vent was inserted. Postoperatively the arterial line waveform remained non-pulsatile.
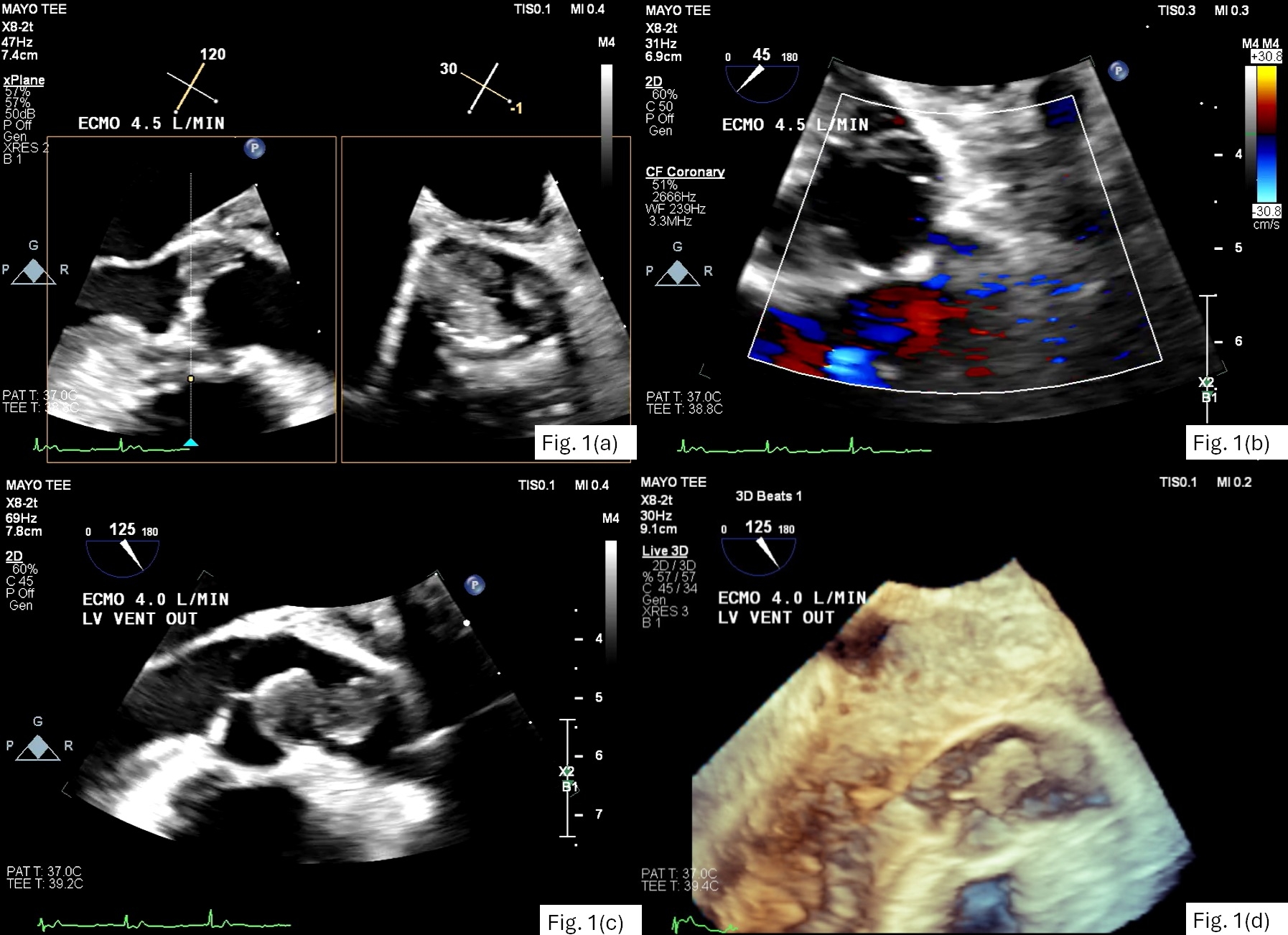
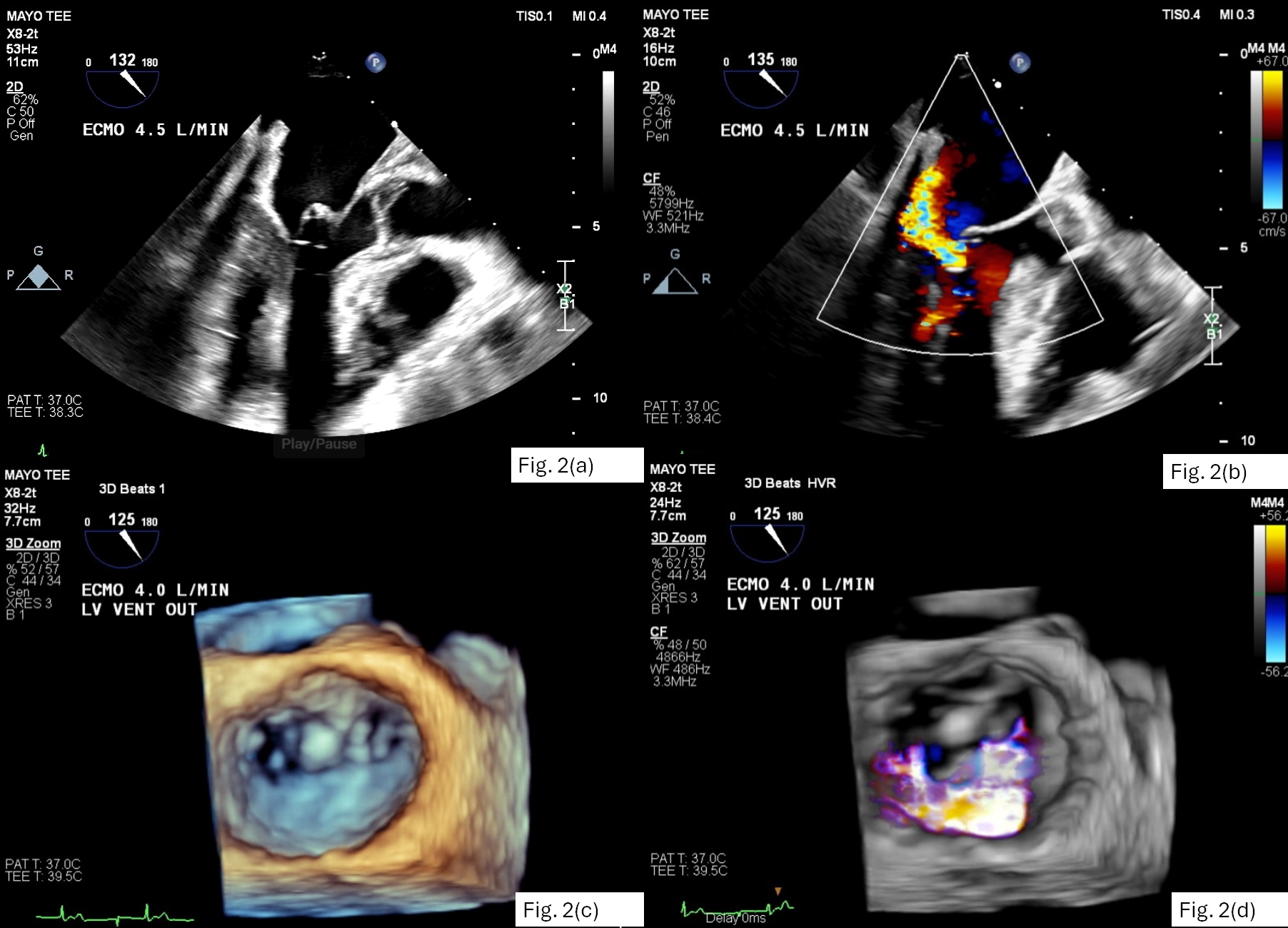
The patient was brought to the OR for mediastinal debridement and removal of the LV vent for the purpose of assessing ventricular function and improving arterial pulsatility. Pulse pressure remained negligible at an ECMO flow of 4.5 L/min. Transeosphageal echocardiography (TEE) demonstrated extensive thrombosis of the aortic root, particularly involving the right and non-coronary sinuses (Fig 1a). The aortic valve (AV) did not open. Patency of the left main coronary ostium was evident by color Doppler (Fig 1b) although no right coronary artery (RCA) flow could be visualized. The tip of LV vent was seen tenting the anterior leaflet of mitral valve (MV) causing significant regurgitation. (Fig. 2a-d)
After vent removal, LV contraction gradually increased and the AV began to open. This progressively dislodged thrombus from the aortic root. At the conclusion of imaging, there was a highly mobile, bi-lobed thrombus attached to the sinotubular junction (Fig 1c-d). Right ventricular (RV) function remained severely reduced. Moderate mitral regurgitation persisted, arising from A2 leaflet prolapse.
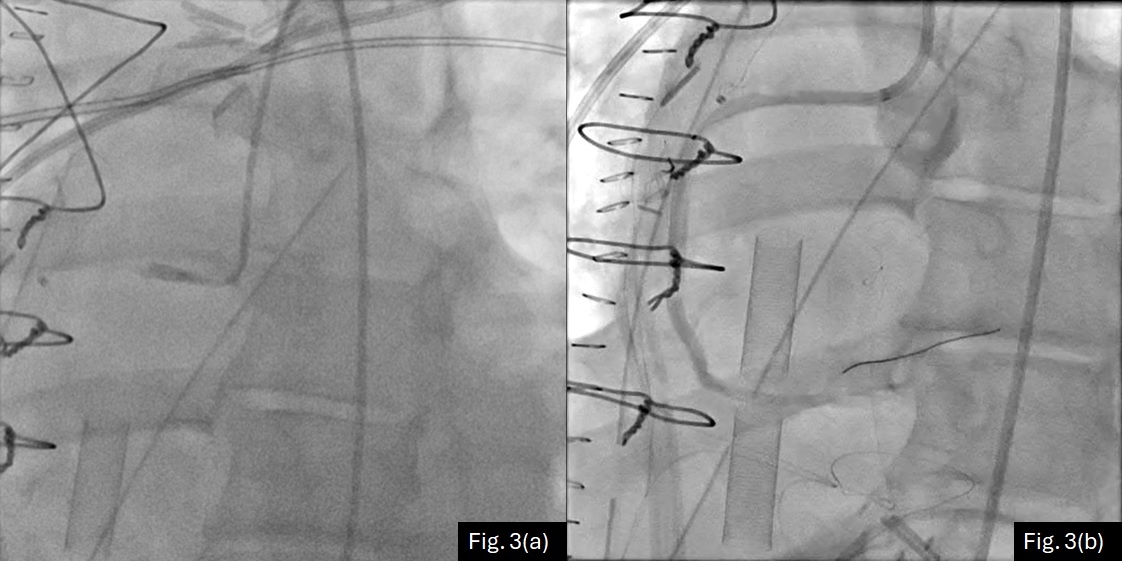
This patient subsequently underwent transcatheter thrombectomy and aspiration of the aortic root with cerebral protection device. Coronary angiogram confirmed proximal RCA occlusion (Fig. 3). Attempts to remove RCA thrombus were only partially successful. She eventually required a second heart transplant due to RV infarction.
Discussion:
This case illustrates a TEE-detected complication of excessive LV venting during VA-ECMO support, namely aortic root thrombosis associated with lack of AV opening. TEE also demonstrated the associated complications of RCA occlusion and iatrogenic mitral valve injury. Unfortunately, these complications were not detected soon enough to avoid RV infarction.
The patient was brought to the OR for mediastinal debridement and removal of the LV vent for the purpose of assessing ventricular function and improving arterial pulsatility. Pulse pressure remained negligible at an ECMO flow of 4.5 L/min. Transeosphageal echocardiography (TEE) demonstrated extensive thrombosis of the aortic root, particularly involving the right and non-coronary sinuses (Fig 1a). The aortic valve (AV) did not open. Patency of the left main coronary ostium was evident by color Doppler (Fig 1b) although no right coronary artery (RCA) flow could be visualized. The tip of LV vent was seen tenting the anterior leaflet of mitral valve (MV) causing significant regurgitation. (Fig. 2a-d)
After vent removal, LV contraction gradually increased and the AV began to open. This progressively dislodged thrombus from the aortic root. At the conclusion of imaging, there was a highly mobile, bi-lobed thrombus attached to the sinotubular junction (Fig 1c-d). Right ventricular (RV) function remained severely reduced. Moderate mitral regurgitation persisted, arising from A2 leaflet prolapse.
This patient subsequently underwent transcatheter thrombectomy and aspiration of the aortic root with cerebral protection device. Coronary angiogram confirmed proximal RCA occlusion (Fig. 3). Attempts to remove RCA thrombus were only partially successful. She eventually required a second heart transplant due to RV infarction.
Discussion:
This case illustrates a TEE-detected complication of excessive LV venting during VA-ECMO support, namely aortic root thrombosis associated with lack of AV opening. TEE also demonstrated the associated complications of RCA occlusion and iatrogenic mitral valve injury. Unfortunately, these complications were not detected soon enough to avoid RV infarction.
More abstracts on this topic:
Decompensated Heart Failure Secondary to a Non-Coronary Sinus of Valsalva to Right Atrium Fistula: A Case Report
Hasan Muhammad, Lavoie Melanie
A distinct clot transcriptomic signature is associated with atrial fibrillation-derived ischemic stroke in the INSIGHT RegistrySeah Carina, Rivet Dennis, Fraser Justin, Kellner Christopher, Devarajan Alex, Vicari James, Dabney Alan, Baltan Selva, Sohrabji Farida, Pennypacker Keith, Nanda Ashish, Woodward Britton