Final ID: MP2066
Guideline-Directed Medical Therapy and Clinical Outcomes in African American Women with Congestive Heart Failure from Low- to Medium-Income Backgrounds at a Safety Net Hospital
Abstract Body (Do not enter title and authors here): Background: Heart failure among African American women represents a significant public health challenge. The high prevalence of comorbidities often necessitates selective implementation of guideline-directed medical therapy (GDMT). This study examines which medication classes should be prioritized in this vulnerable population.
Methods: We conducted a retrospective study of 283 African American women with heart failure admitted to Cape Fear Valley Medical Center, a safety-net hospital serving low-income patients in North Carolina (2021-2022). We analyzed relationships between GDMT regimens and clinical outcomes.
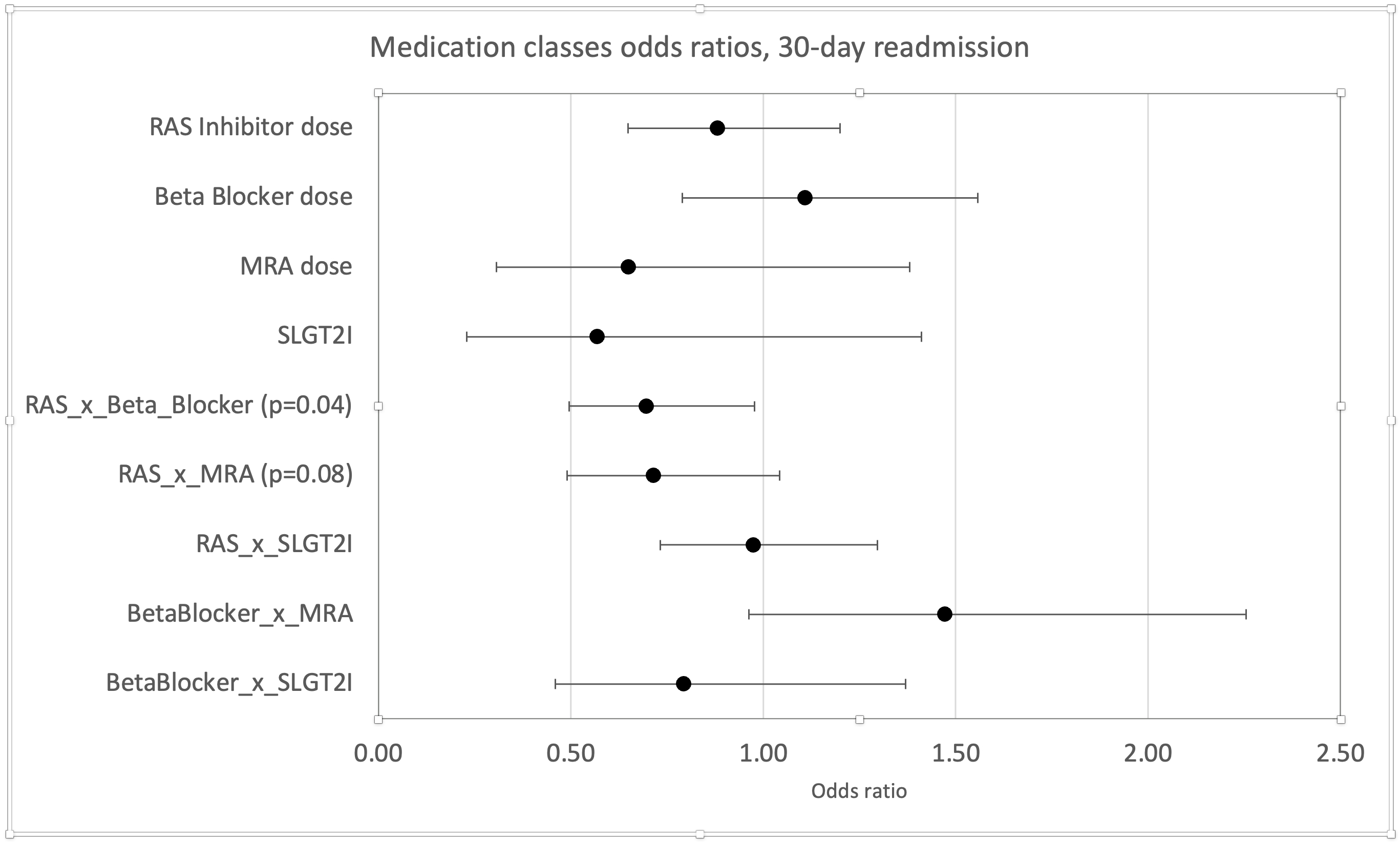
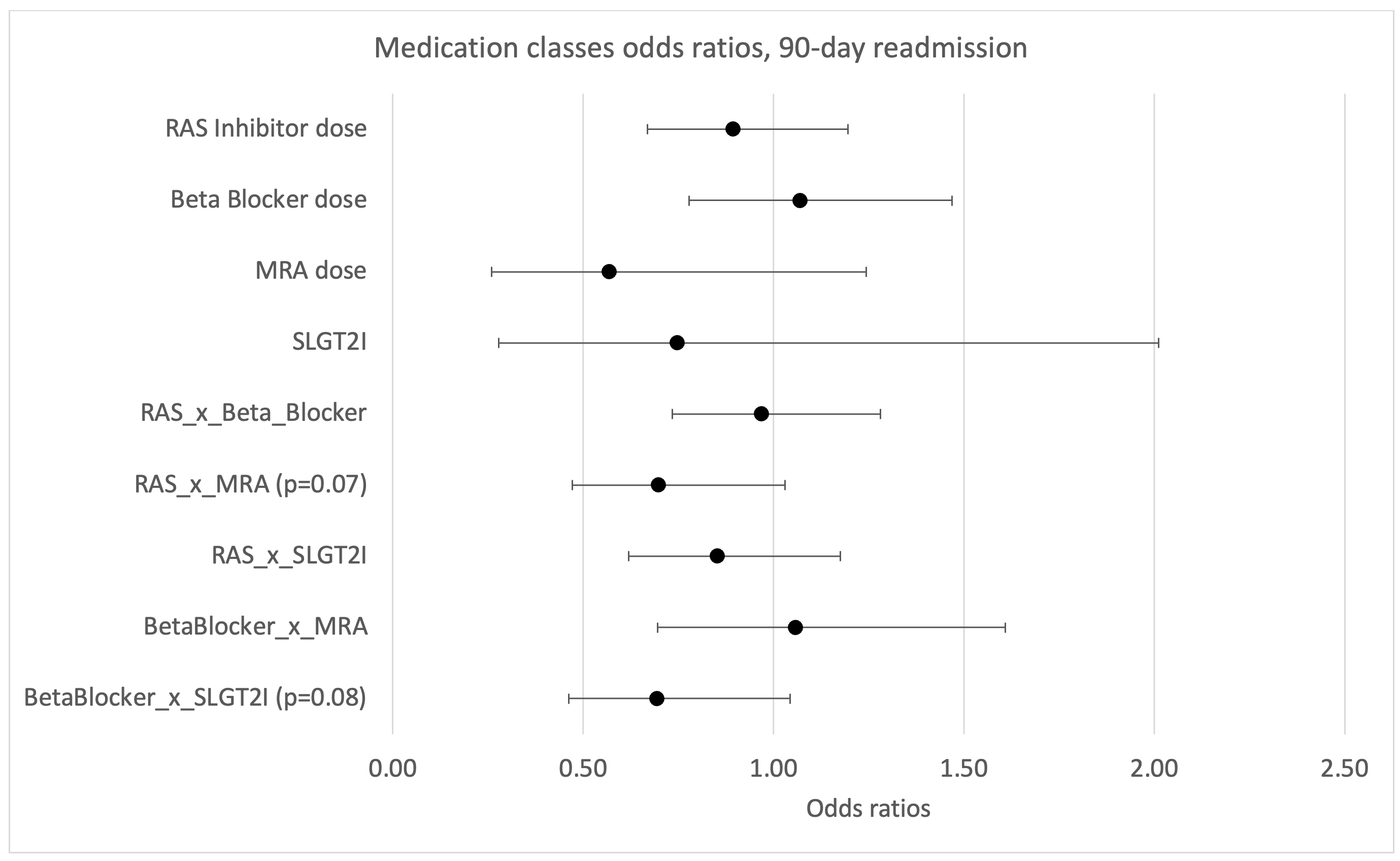
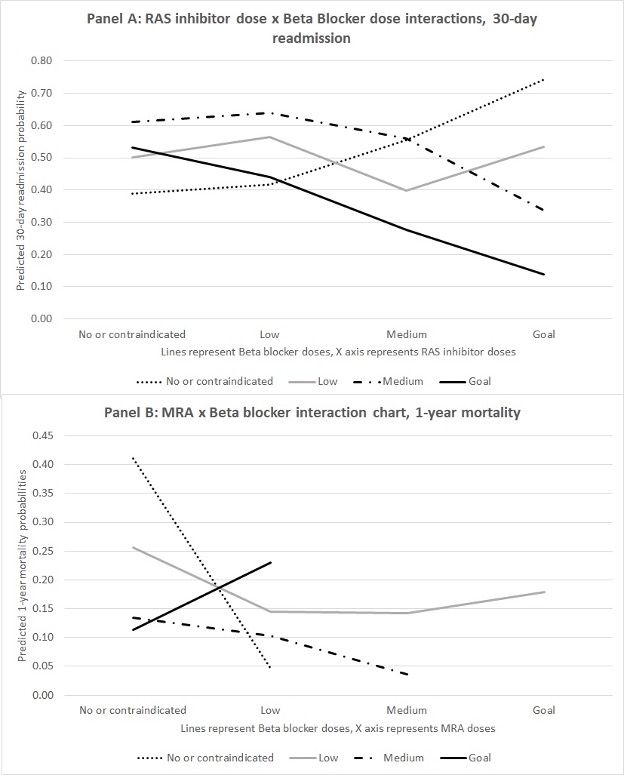
Results: Among patients, 50% experienced 30-day readmission, 57% 90-day readmission, and 23% died within 1 year. Medication utilization was suboptimal: 10% received goal doses of RAS inhibitors, 13% goal doses of beta blockers, 4% medium/goal doses of mineralocorticoid receptor antagonists (MRAs), and 11% SGLT2 inhibitors. Mean GDMT composite was 2.4±1.8, with only 8% achieving composite ≥5. Each one-point increase in GDMT composite reduced 30-day (OR=0.85, p=0.02) and 90-day readmission risk (OR=0.86, p=0.03). Higher GDMT composite was associated with decreased mortality in unadjusted analysis (OR=0.86, p=0.07). Concurrent optimization of RAS inhibitors and beta blockers reduced readmission risk (OR=0.70, p=0.04). Low-dose MRA lowered 30-day readmission (OR=0.27, p<0.01). Medium-dose beta blockers reduced 1-year mortality (OR=0.13, p=0.03), as did medium doses of MRA (OR<0.01, p<0.01).
Conclusions: Strategic prioritization of specific GDMT components improves outcomes in this population with multiple comorbidities. Each one-point increase in GDMT composite was associated with 15% reduced readmission risk. Beta blockers should be prioritized for mortality reduction, MRAs for both mortality and readmission reduction, and RAS inhibitors with beta blockers for reducing readmissions.
Methods: We conducted a retrospective study of 283 African American women with heart failure admitted to Cape Fear Valley Medical Center, a safety-net hospital serving low-income patients in North Carolina (2021-2022). We analyzed relationships between GDMT regimens and clinical outcomes.
Results: Among patients, 50% experienced 30-day readmission, 57% 90-day readmission, and 23% died within 1 year. Medication utilization was suboptimal: 10% received goal doses of RAS inhibitors, 13% goal doses of beta blockers, 4% medium/goal doses of mineralocorticoid receptor antagonists (MRAs), and 11% SGLT2 inhibitors. Mean GDMT composite was 2.4±1.8, with only 8% achieving composite ≥5. Each one-point increase in GDMT composite reduced 30-day (OR=0.85, p=0.02) and 90-day readmission risk (OR=0.86, p=0.03). Higher GDMT composite was associated with decreased mortality in unadjusted analysis (OR=0.86, p=0.07). Concurrent optimization of RAS inhibitors and beta blockers reduced readmission risk (OR=0.70, p=0.04). Low-dose MRA lowered 30-day readmission (OR=0.27, p<0.01). Medium-dose beta blockers reduced 1-year mortality (OR=0.13, p=0.03), as did medium doses of MRA (OR<0.01, p<0.01).
Conclusions: Strategic prioritization of specific GDMT components improves outcomes in this population with multiple comorbidities. Each one-point increase in GDMT composite was associated with 15% reduced readmission risk. Beta blockers should be prioritized for mortality reduction, MRAs for both mortality and readmission reduction, and RAS inhibitors with beta blockers for reducing readmissions.
More abstracts on this topic:
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulin
Dabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey
Beta-Blocker Efficacy in Acute Myocardial Infarction: A Machine Learning Approach using the KAMIR-NIH DatasetRha Seung-woon, Park Chang Gyu, Oh Dong Joo, Cha Jinah, Ahn Woo Jin, Hyun Sujin, Choi Se Yeon, Choi Byoung Geol, Sinurat Markz, Park Soohyung, Choi Cheol Ung