Final ID: MP1260
Health at a Distance: Urban-Rural Disparities in Hypertensive Emergency
Abstract Body (Do not enter title and authors here): Introduction/background: Rural hospital closures and limited access to subspecialty care may adversely affect outcomes for patients with hypertensive emergencies—a growing cause of hospitalization in the U.S. This study compared clinical outcomes and healthcare utilization between rural and urban hospitalizations for hypertensive emergency.
Methods: Cross-sectional study using 2022 National Inpatient Sample (NIS), a nationally representative, all-payer database of U.S. hospitalizations. Adults hospitalized with a principal diagnosis of hypertensive emergency (ICD-10: I16.1) were included. Hospital rurality was categorized using Core-Based Statistical Area definitions. Primary outcomes included in-hospital mortality, length of stay (LOS), and total hospitalization charges. Multivariable logistic and linear regression models adjusted for age, payer status, Charlson Comorbidity Index (CCI), income quartile, and hospital region and teaching status. Survey weights were applied to generate nationally representative estimates.
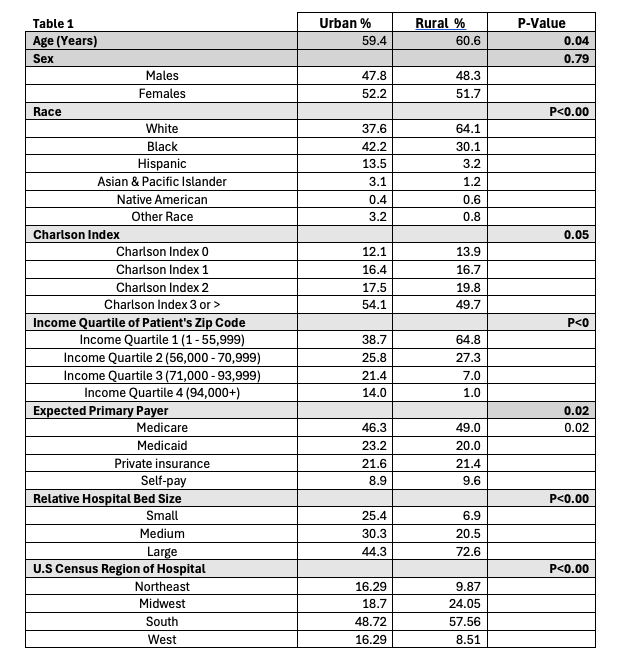
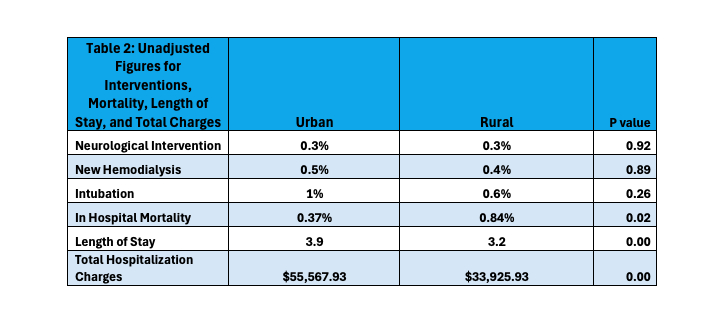
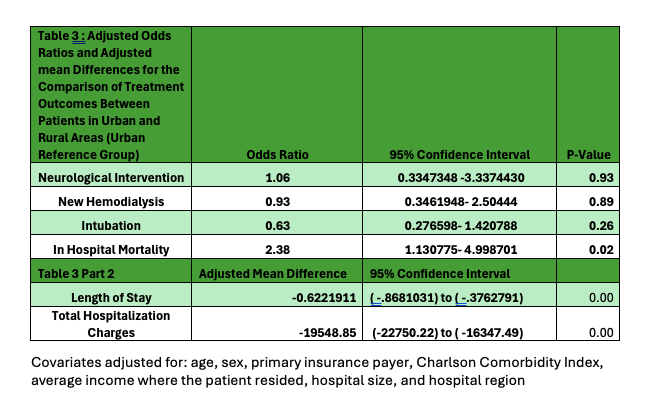
Results: Of 70,155 hospitalizations (mean age [SD]: 59.5 [0.3] years; 47.8% male; 39.4% White), 6.78% occurred in rural hospitals. The mean charge was $54,091 [$1,700], and LOS was 3.9 [0.09] days. Compared to urban patients, rural patients were older (60.6 [1.1] vs. 59.4 [0.3] years), more likely to be White (64.1% vs. 37.6%), Medicare-covered (49.0% vs. 46.3%), and from lower-income areas (64.8% vs. 38.7% in the lowest income quartile) (all p<0.01). Rural patients had a lower comorbidity burden (CCI ≥3: 49.7% vs. 54.1%). Unadjusted analyses showed higher in-hospital mortality in rural (0.84% vs. 0.37%), shorter LOS (3.2 vs. 3.9 days), and lower hospital charges ($33,926 vs. $55,568; all p<0.001). Rates of critical interventions, including neurological procedures (0.30% vs. 0.30%), renal replacement therapy (0.4% vs. 0.5%), and intubation (0.6% vs. 1.0%), were similar (all p>0.30). After adjustments, rural hospitalizations remained associated with higher in-hospital death (aOR 2.38; 95% CI, 1.13–5.00), shorter LOS (−0.62 days; 95% CI, −0.85 to −0.39), and lower hospitalization charges (−$19,549; 95% CI, −$25,000 to −$14,000).
Conclusion: Rural hospitalizations for hypertensive emergency are marked by higher mortality despite lower illness burden and significantly lower resource utilization. These disparities highlight the need for targeted strategies to strengthen critical care infrastructure and improve equity in rural health systems.
Methods: Cross-sectional study using 2022 National Inpatient Sample (NIS), a nationally representative, all-payer database of U.S. hospitalizations. Adults hospitalized with a principal diagnosis of hypertensive emergency (ICD-10: I16.1) were included. Hospital rurality was categorized using Core-Based Statistical Area definitions. Primary outcomes included in-hospital mortality, length of stay (LOS), and total hospitalization charges. Multivariable logistic and linear regression models adjusted for age, payer status, Charlson Comorbidity Index (CCI), income quartile, and hospital region and teaching status. Survey weights were applied to generate nationally representative estimates.
Results: Of 70,155 hospitalizations (mean age [SD]: 59.5 [0.3] years; 47.8% male; 39.4% White), 6.78% occurred in rural hospitals. The mean charge was $54,091 [$1,700], and LOS was 3.9 [0.09] days. Compared to urban patients, rural patients were older (60.6 [1.1] vs. 59.4 [0.3] years), more likely to be White (64.1% vs. 37.6%), Medicare-covered (49.0% vs. 46.3%), and from lower-income areas (64.8% vs. 38.7% in the lowest income quartile) (all p<0.01). Rural patients had a lower comorbidity burden (CCI ≥3: 49.7% vs. 54.1%). Unadjusted analyses showed higher in-hospital mortality in rural (0.84% vs. 0.37%), shorter LOS (3.2 vs. 3.9 days), and lower hospital charges ($33,926 vs. $55,568; all p<0.001). Rates of critical interventions, including neurological procedures (0.30% vs. 0.30%), renal replacement therapy (0.4% vs. 0.5%), and intubation (0.6% vs. 1.0%), were similar (all p>0.30). After adjustments, rural hospitalizations remained associated with higher in-hospital death (aOR 2.38; 95% CI, 1.13–5.00), shorter LOS (−0.62 days; 95% CI, −0.85 to −0.39), and lower hospitalization charges (−$19,549; 95% CI, −$25,000 to −$14,000).
Conclusion: Rural hospitalizations for hypertensive emergency are marked by higher mortality despite lower illness burden and significantly lower resource utilization. These disparities highlight the need for targeted strategies to strengthen critical care infrastructure and improve equity in rural health systems.
More abstracts on this topic:
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART study
Reitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas
A durable reduction in blood pressure by ultrasound renal denervation: A real-world, single center experienceKing Jordan, Gharib Wissam