Final ID: MP1985
Impact of frailty on in-hospital outcome of STEMI hospitalization: Analysis of National Inpatient Sample
Abstract Body (Do not enter title and authors here): Background and Purpose: National data and trends on the impact of frailty on ST-segment elevation myocardial infarction (STEMI) are lacking.
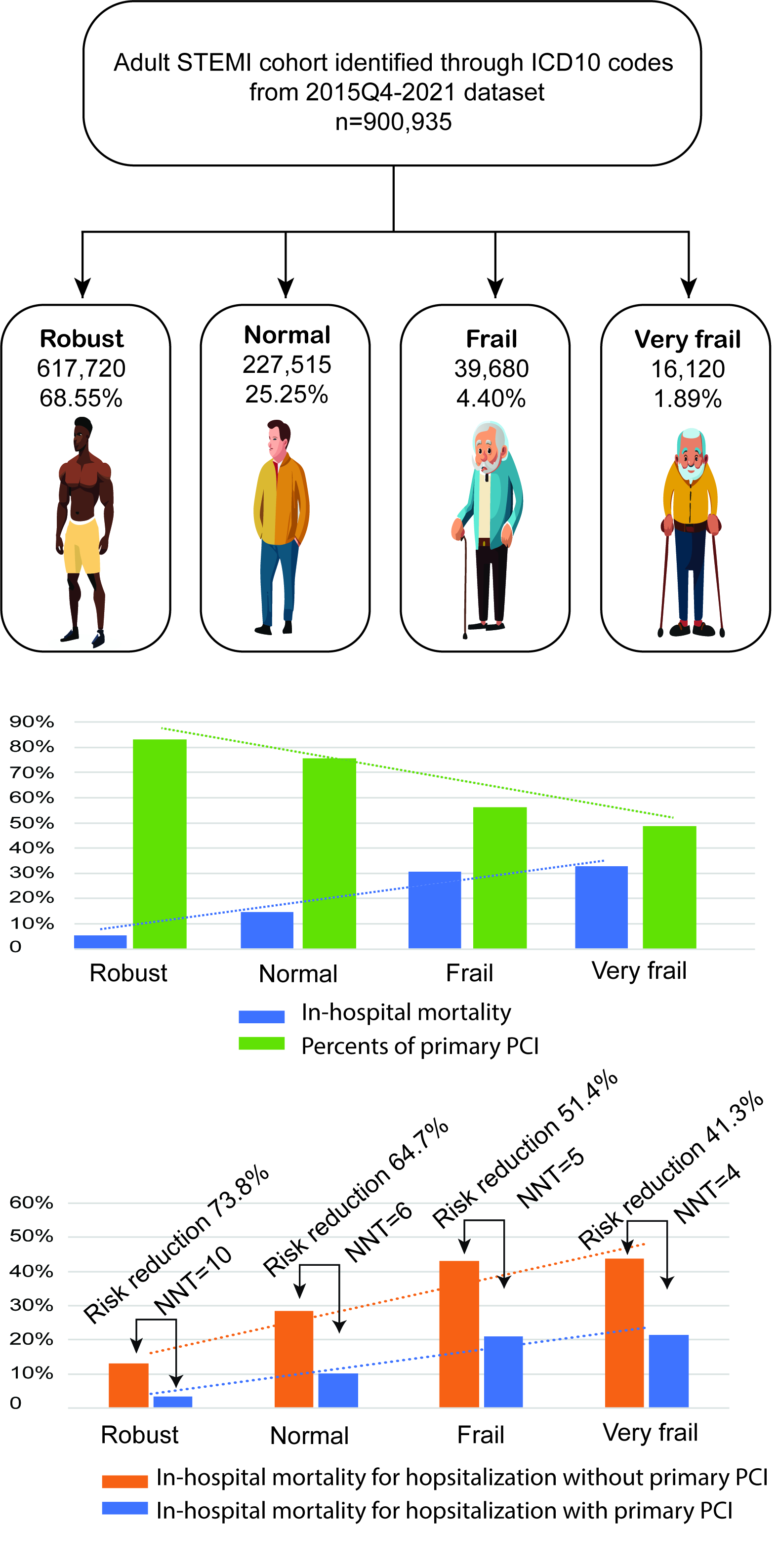
Methods: Retrospective data were extracted from the United States National Inpatient Sample from October 2015 to 2021 for hospitalizations with a STEMI diagnosis. A total of 900,935 STEMI hospitalizations were included in the final cohort. Based on Risk Analysis Index (RAI) scores, hospitalizations are categorized into robust, normal, frail, and very frail groups.
Results: Frail and very frail hospitalizations account for about 6% of total hospitalizations. The in-hospital mortality rates for robust, normal, frail, and very frail are 5.09%, 14.49%, 30.67%, and 32.88%, respectively. Compared to robust and normal hospitalizations, Frail and very frail hospitalizations are less likely to receive primary percutaneous coronary intervention (pPCI).
For overall hospitalizations, the odds ratios for in-hospital mortality for pPCI treated robust, normal, frail, and very frail hospitalizations are 0.23 [95% CI (0.22-0.25)]; p<0.001, 0.28 [95% CI (0.27-0.30)]; p<0.001, 0.34 [95% CI (0.30-0.37)]; p<0.001, and 0.35 [95% CI (0.30-0.42)]; p<0.001, respectively. The reduction of in-hospital mortality with pPCI treatment is consistent after propensity score matching for each frailty groups. Fewer patients need to be treated to prevent one additional in-hospital death in the frail and very frail groups compared to the robust and normal groups (number needed to treat (NNT)=4 in the very frail group and NNT=5 in frail group, whereas NNT =10 in the robust group).
Conclusions: This analysis highlights the worse in-hospital outcomes of frail and very frail hospitalizations for STEMI patients. Despite the fact that pPCI consistently shows a significant reduction in in-hospital mortality. frail and very frail hospitalizations are less likely to receive this treatment. This underscores the need for careful consideration of frailty in treatment decisions, as timely pPCI may improve outcomes even in these high-risk population.
Methods: Retrospective data were extracted from the United States National Inpatient Sample from October 2015 to 2021 for hospitalizations with a STEMI diagnosis. A total of 900,935 STEMI hospitalizations were included in the final cohort. Based on Risk Analysis Index (RAI) scores, hospitalizations are categorized into robust, normal, frail, and very frail groups.
Results: Frail and very frail hospitalizations account for about 6% of total hospitalizations. The in-hospital mortality rates for robust, normal, frail, and very frail are 5.09%, 14.49%, 30.67%, and 32.88%, respectively. Compared to robust and normal hospitalizations, Frail and very frail hospitalizations are less likely to receive primary percutaneous coronary intervention (pPCI).
For overall hospitalizations, the odds ratios for in-hospital mortality for pPCI treated robust, normal, frail, and very frail hospitalizations are 0.23 [95% CI (0.22-0.25)]; p<0.001, 0.28 [95% CI (0.27-0.30)]; p<0.001, 0.34 [95% CI (0.30-0.37)]; p<0.001, and 0.35 [95% CI (0.30-0.42)]; p<0.001, respectively. The reduction of in-hospital mortality with pPCI treatment is consistent after propensity score matching for each frailty groups. Fewer patients need to be treated to prevent one additional in-hospital death in the frail and very frail groups compared to the robust and normal groups (number needed to treat (NNT)=4 in the very frail group and NNT=5 in frail group, whereas NNT =10 in the robust group).
Conclusions: This analysis highlights the worse in-hospital outcomes of frail and very frail hospitalizations for STEMI patients. Despite the fact that pPCI consistently shows a significant reduction in in-hospital mortality. frail and very frail hospitalizations are less likely to receive this treatment. This underscores the need for careful consideration of frailty in treatment decisions, as timely pPCI may improve outcomes even in these high-risk population.
More abstracts on this topic:
Assessing Coronary Artery Disease Severity: Leveraging Inflammatory Markers As a Prognostic Indicators
Turnbull Scott, Dugal Jasmine, Gill Randeep, Wang Shawn, Cross Chad, Mubder Mohamad
Acute Exposure to High PM2.5 Levels Increases the Risk of Late All-Cause Mortality in Patients with STEMIFathieh Sina, Tran Hao, Faour Amir, Pahn Reece, Long Mitchell, Tam Gladys, Figtree Gemma, Negishi Kazuaki, French John