Final ID: MDP956
Resource Utilization and Short-term Readmissions After Implantation of Left Ventricular Assist Devices and Heart Transplantations in Adults in the United States – A Contemporary Insight from the National Readmission Database: 2018 - 2021
Abstract Body (Do not enter title and authors here):
Introduction: Heart transplants (HT) and left ventricular assist devices (LVADs) are treatment options for advanced heart failure refractory to standard therapy. Historically, LVADs have been used as either destination therapy or a bridge to transplant. However, recent changes to the organ allocation system have deprioritized patients on LVADs as transplant recipients, leading to divisive views on the role of an LVAD. We sought to describe outcomes with each modality, highlighting each option's strengths and clinical utility.
Aim: To assess costs related to index hospitalization, 30-day (30DRC) and 90-day (90DRC) readmission categories for both subgroups.
Method: We analyzed the National Readmission Database (NRD) from January 1, 2018, to December 31, 2021, identifying patients with HT and LVAD via ICD-10-CM codes. We selected this recent time frame to limit the influence of older LVAD technology and heart allocation schemes. We excluded patients <18 and patients with HT and LVAD during the index hospitalization. The primary outcomes were 30-day and 90-day readmission rates after index hospital discharge. Secondary outcomes included the cost of hospitalization during the index hospitalization and readmissions.
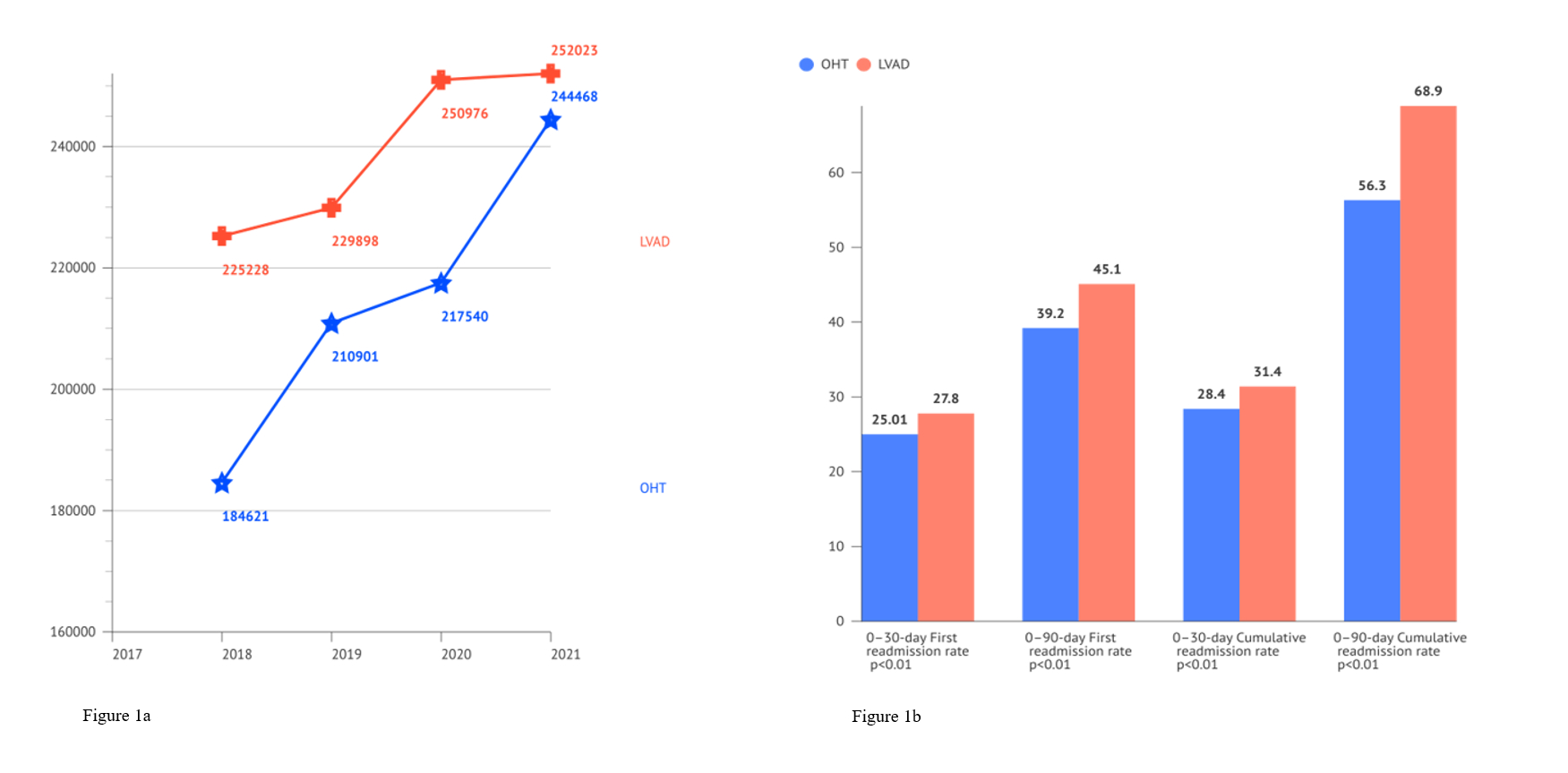
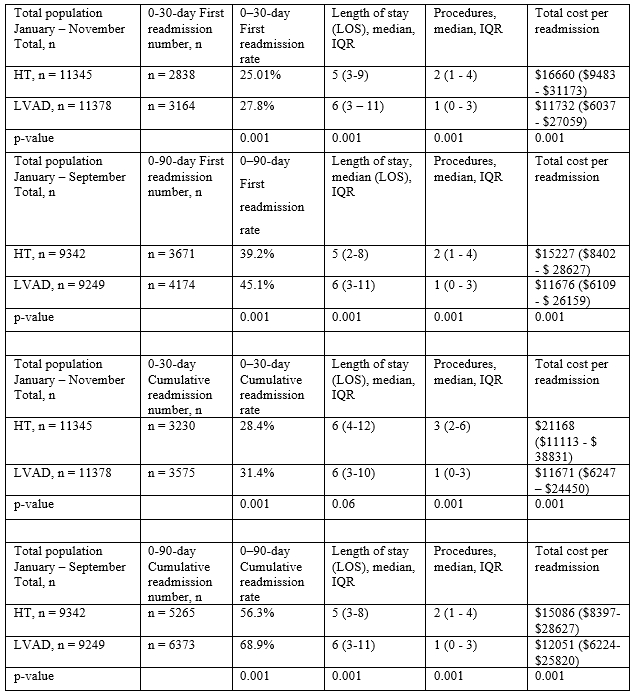
Results: We identified 27,308 weighted index hospital admissions from January to December 2018-2021; LVAD was implanted in 14295 (52.4%). The median index admission cost is lower in the HT subgroup than in the LVAD subgroup across all studied years (Figure 1a). Both groups, however, show an increase in median costs from 2018 to 2021, with an 11.8% rise in the LVAD subgroup and a 32.42% rise in the HT subgroup. In the 30DRC, we identified 22,723 index hospitalizations, of which 11378 (50.07%) were LVAD recipients. LVAD recipients were significantly more likely to be hospitalized within 30 days (3164, 27.8% vs 2838, 25.01%; p=0.001). However, the HT group had higher readmission costs [$16660 ($9483 - $31173) vs$11732 ($6037 - $27059)), p=0.001]. Similar findings were noted in the 90DRC group (Figure 1b and Figure 2).
Conclusion:
Both LVAD and HT had comparable burdens on resource and short-term rehospitalization risk. Index hospitalization costs were higher for the LVAD group, whereas HT was associated with higher readmission-related costs.
Introduction: Heart transplants (HT) and left ventricular assist devices (LVADs) are treatment options for advanced heart failure refractory to standard therapy. Historically, LVADs have been used as either destination therapy or a bridge to transplant. However, recent changes to the organ allocation system have deprioritized patients on LVADs as transplant recipients, leading to divisive views on the role of an LVAD. We sought to describe outcomes with each modality, highlighting each option's strengths and clinical utility.
Aim: To assess costs related to index hospitalization, 30-day (30DRC) and 90-day (90DRC) readmission categories for both subgroups.
Method: We analyzed the National Readmission Database (NRD) from January 1, 2018, to December 31, 2021, identifying patients with HT and LVAD via ICD-10-CM codes. We selected this recent time frame to limit the influence of older LVAD technology and heart allocation schemes. We excluded patients <18 and patients with HT and LVAD during the index hospitalization. The primary outcomes were 30-day and 90-day readmission rates after index hospital discharge. Secondary outcomes included the cost of hospitalization during the index hospitalization and readmissions.
Results: We identified 27,308 weighted index hospital admissions from January to December 2018-2021; LVAD was implanted in 14295 (52.4%). The median index admission cost is lower in the HT subgroup than in the LVAD subgroup across all studied years (Figure 1a). Both groups, however, show an increase in median costs from 2018 to 2021, with an 11.8% rise in the LVAD subgroup and a 32.42% rise in the HT subgroup. In the 30DRC, we identified 22,723 index hospitalizations, of which 11378 (50.07%) were LVAD recipients. LVAD recipients were significantly more likely to be hospitalized within 30 days (3164, 27.8% vs 2838, 25.01%; p=0.001). However, the HT group had higher readmission costs [$16660 ($9483 - $31173) vs$11732 ($6037 - $27059)), p=0.001]. Similar findings were noted in the 90DRC group (Figure 1b and Figure 2).
Conclusion:
Both LVAD and HT had comparable burdens on resource and short-term rehospitalization risk. Index hospitalization costs were higher for the LVAD group, whereas HT was associated with higher readmission-related costs.
More abstracts on this topic:
A Bridge from Sweet to Sour: A Case of Recurrent Myocardial Stunning in Diabetic Ketoacidosis
Satish Vikyath, Pargaonkar Sumant, Slipczuk Leandro, Schenone Aldo, Maliha Maisha, Chi Kuan Yu, Sunil Kumar Sriram, Borkowski Pawel, Vyas Rhea, Rodriguez Szaszdi David Jose Javier, Kharawala Amrin, Seo Jiyoung
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint InhibitorPatel Romil, Hussain Kifah, Gordon Robert