Final ID: MDP1389
In hospital Outcomes of Acute Myocarditis in Adults with Systemic Inflammatory Disease: A Population-based Analysis in The United States
Abstract Body (Do not enter title and authors here): Systemic inflammatory diseases (SID) are associated with adverse cardiovascular (CV) events, due to derangement in innate immunity. Understanding the association with acute myocarditis (AMC) is crucial for preemptive management strategies and improving patient outcomes.
Methods:
We identified and compared adults (>18 years) with SID vs. non-SID patients hospitalized with AMC using the National In-patient sample database from 2016-2020. Six SID were selected based on HLA antigen distribution. The risks of all-cause mortality and major adverse cardiac and cerebrovascular events (CVA, cardiac arrest, acute heart failure (AHF), Ventricular arrhythmia, complete AV block, AMI, and PCI), and use of mechanical circulatory support (MCS) were assessed in adult AMC admissions with and without SID. SID were divided into 6 cohorts: SLE, RA, psoriasis (PS), IBD, Hashimoto thyroiditis (HT), and multiple sclerosis (MS) subgroups.
Results:
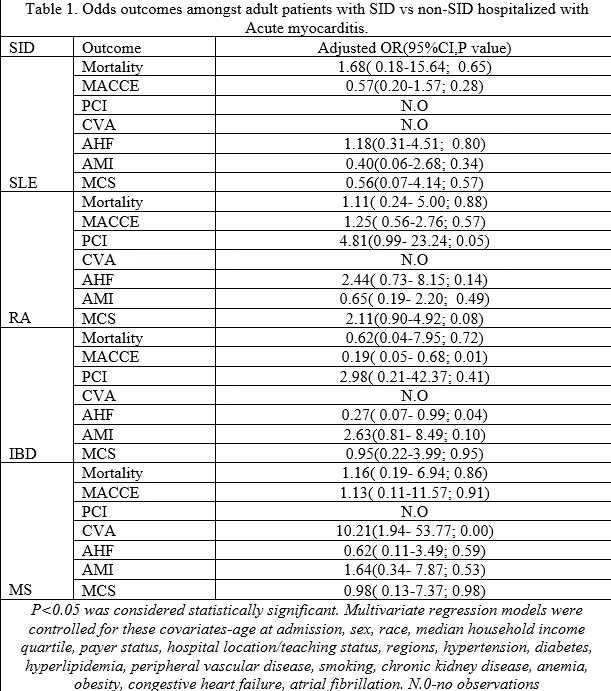
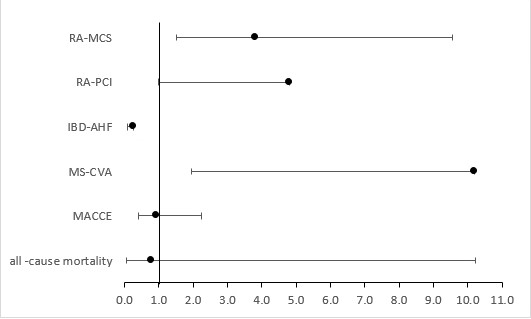
Overall adults AMC admissions were 26,475. The rate of AMC in non-SID was 96%. Mean age of non-SID were similar in 4 cohorts, but relatively older in RA subgroup (47.5 vs 61.5 years). We observed male predominance in the PS vs IBD groups (62% vs 51% vs 63%), but more females in the SLE, RA, HT, and MS cohort. We observed comparable mortality (aOR 1.425; CI 0.062-10.23 p=0.862) and MACE (aOR 0.943; CI 0.398-2.231 p=0.894) rates across all studied subgroups. The RA-AMC cohort had significantly higher odds of MCS use (aOR 3.8; CI 1.52- 9.55, p=0.004), after adjusting for significant confounders. The IBD-AMC cohort had significantly reduced odds of AHF (aOR 0.28; CI 0.076 - 0.99, p=0.04). However, the odds of AMI and VA were not statistically significant.(Table 1)
Conclusions:
The RA-AMC cohort are about 4 times more likely to require mechanical circulatory support during hospitalization for acute myocarditis, while IBD-AMC are less likely to have AHF. Prospective studies would be required to further examine the cardiovascular outcome in this cohort. Prospective studies would be required to further examine the cardovascular outcomes in this cohort.
Methods:
We identified and compared adults (>18 years) with SID vs. non-SID patients hospitalized with AMC using the National In-patient sample database from 2016-2020. Six SID were selected based on HLA antigen distribution. The risks of all-cause mortality and major adverse cardiac and cerebrovascular events (CVA, cardiac arrest, acute heart failure (AHF), Ventricular arrhythmia, complete AV block, AMI, and PCI), and use of mechanical circulatory support (MCS) were assessed in adult AMC admissions with and without SID. SID were divided into 6 cohorts: SLE, RA, psoriasis (PS), IBD, Hashimoto thyroiditis (HT), and multiple sclerosis (MS) subgroups.
Results:
Overall adults AMC admissions were 26,475. The rate of AMC in non-SID was 96%. Mean age of non-SID were similar in 4 cohorts, but relatively older in RA subgroup (47.5 vs 61.5 years). We observed male predominance in the PS vs IBD groups (62% vs 51% vs 63%), but more females in the SLE, RA, HT, and MS cohort. We observed comparable mortality (aOR 1.425; CI 0.062-10.23 p=0.862) and MACE (aOR 0.943; CI 0.398-2.231 p=0.894) rates across all studied subgroups. The RA-AMC cohort had significantly higher odds of MCS use (aOR 3.8; CI 1.52- 9.55, p=0.004), after adjusting for significant confounders. The IBD-AMC cohort had significantly reduced odds of AHF (aOR 0.28; CI 0.076 - 0.99, p=0.04). However, the odds of AMI and VA were not statistically significant.(Table 1)
Conclusions:
The RA-AMC cohort are about 4 times more likely to require mechanical circulatory support during hospitalization for acute myocarditis, while IBD-AMC are less likely to have AHF. Prospective studies would be required to further examine the cardiovascular outcome in this cohort. Prospective studies would be required to further examine the cardovascular outcomes in this cohort.
More abstracts on this topic:
Balloon-Expandable versus Self-Expandable Valve for the Management of Bicuspid Aortic Disease: An Updated Meta-Analysis of Clinical Outcomes
Oliveira Izadora, Graner Moreira Humberto, De Sousa Andre, Paiva Arthur, Ferreira Vitor, De Sá Carlos Eduardo, Alves Alencar Joao Victor, Alves Alencar Pedro Lucas, Duarte Lima Ana Paula, Oliveira Vinicius
ANCA-Negative Eosinophilic Myocarditis Masquerading as STEMI: A Case of Fulminant Cardiogenic ShockBonilla Harrison, Guardia Joshua, Niroula Shailesh, Liranzo Niurka, Tsyngauz Esther