Scientific Sessions 2024
/
Inflammation and ACS
/
Systemic inflammation after STEMI – impact on infarct size and outcome –
Final ID: MDP726
Systemic inflammation after STEMI – impact on infarct size and outcome –
Abstract Body (Do not enter title and authors here): Background: Systemic inflammation due to acute myocardial infarction (MI) leads to leukocyte accumulation inside cardiac tissue. Three days after MI the reparative phase is initiated, where cardiac macrophages adopt anti-inflammatory phenotypes and support scar formation and cardiac healing. Delayed resolution of inflammation leads to adverse cardiac remodeling after MI.
Objective: To correlate persistent inflammation and delayed resolution of inflammation with infarct size and mortality in patients with ST-elevation myocardial infarction (STEMI).
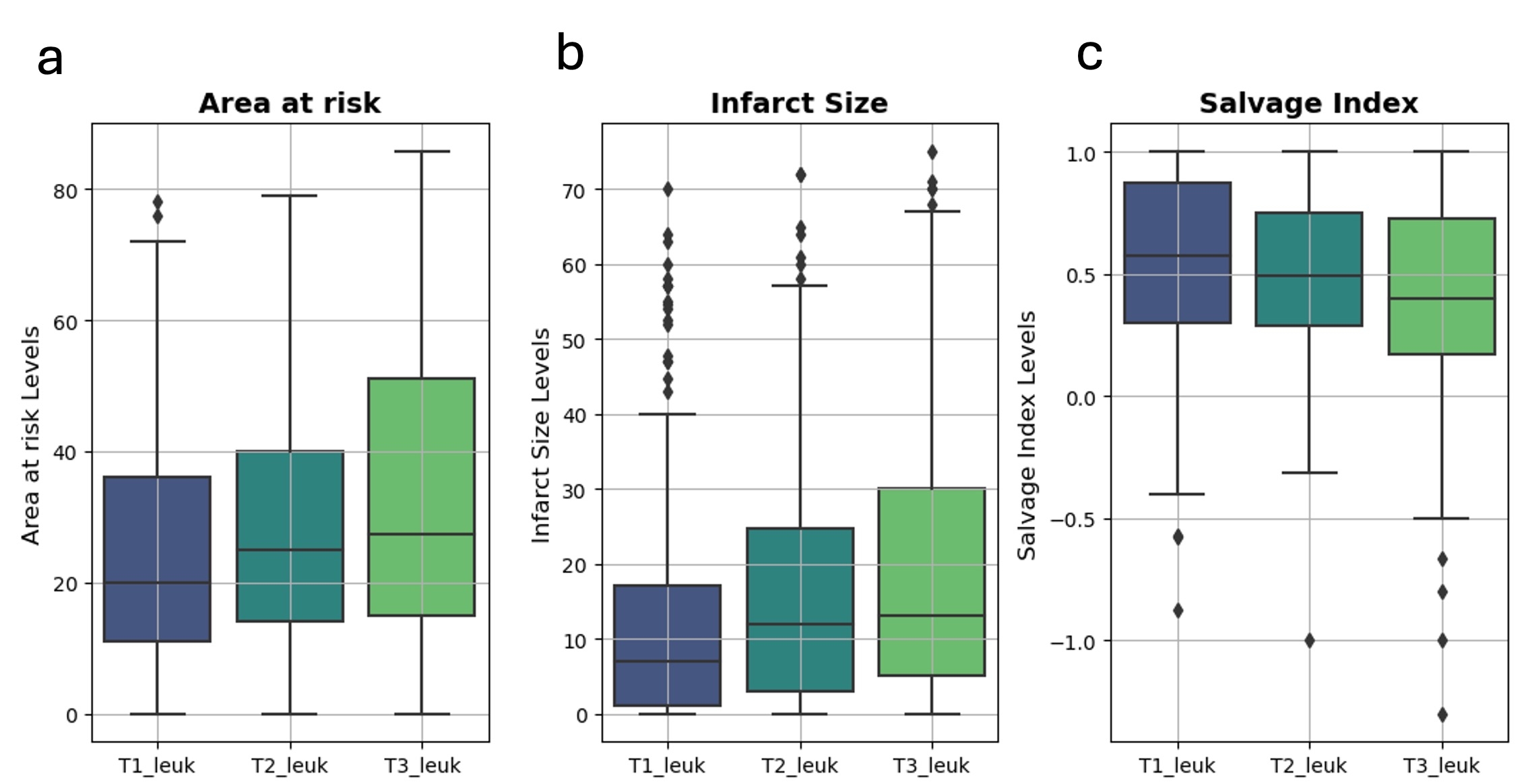
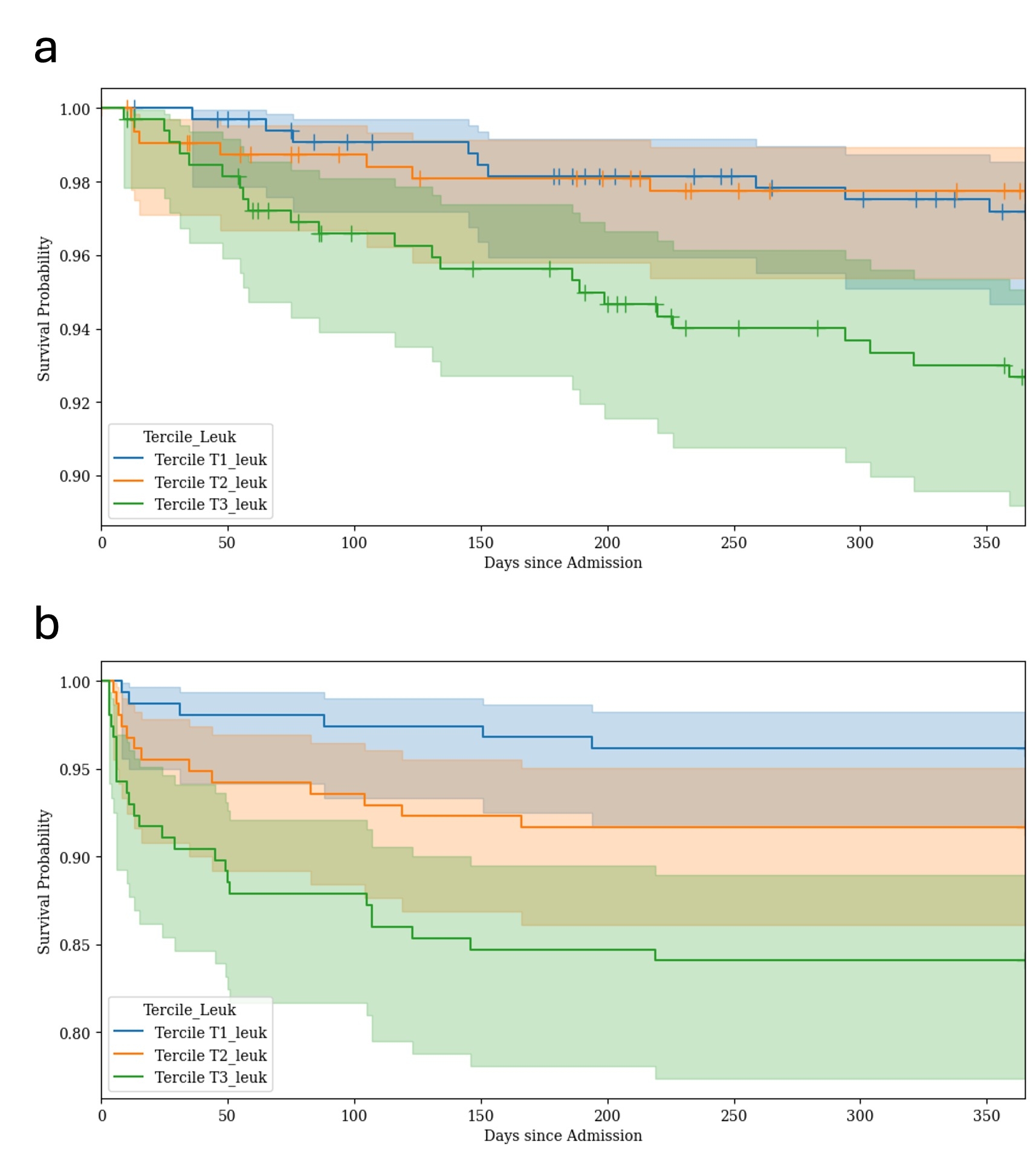
Methods and Results: This retrospective study, included data of STEMI patients treated with primary percutaneous coronary intervention (PPCI) from a historical (n=1155, 2002-2007) and contemporary (n=698, 2014-2022) cohort. Patients were grouped in tertiles according to leukocyte counts on day 3 after MI, as a surrogate parameter for delayed resolution of inflammation. In the historical cohort Serial single-photon emission computerized tomography imaging was available on admission and 7 to 14 days. Patients with elevated leukocyte counts after 72 h (T3 group) showed greatest area at risk (AAR) before PPCI (T1, AAR (median): 20.0% (IQR 11.0–36.0%); T2, AAR (median): 25.0% (IQR 14.0–40.0%), T3, AAR (median): 27.4% (IQR, 15.0–51.0%) and final infarct size (FIS) after 7 to 14 days after MI (T1, FIS (median): 7.0% (IQR 1.0–17.0%); T2, FIS (median): 12.0% (IQR 3.0–24.7%); T3, FIS (median): 13.0% (IQR 5.0–30.0%)) of the left ventricle. In line with these scintigraphic findings, peak creatine kinase myocardial band (CK-MB) values, as an enzymatic estimate of the infarct size, were also highest in T3. Additionally left ventricular ejection fraction (LV-EF) was lowest in the T3. At one year, 8 patients in T1, 7 patients in T2, and 22 patients in T3 had died (Kaplan–Meier estimates of 1-year mortality: 2.6%, 2.3%, and 7.3%, respectively (log-rank test: T1 vs. T3: p=0.01; T2 vs. T3: p=0.03). In the contemporary cohort we also found that patients with elevated leukocyte counts after 72 h (T3 group) showed greatest enzymatic infarct size, estimated by peak CK-MB values and reduced LV-EF. At one year, 6 patients in T1, 13 patients in T2 and 25 patients in T3 had died (Kaplan–Meier estimates of 1-year mortality: 3.8%, 8.3%, and 15.9%, respectively (log-rank test: T1 vs. T3: p<0.005, T2 vs. T3: p=0.004).
Conclusion: Delayed resolution of inflammation following MI, is associated with poorer outcomes at one year in STEMI patients.
Objective: To correlate persistent inflammation and delayed resolution of inflammation with infarct size and mortality in patients with ST-elevation myocardial infarction (STEMI).
Methods and Results: This retrospective study, included data of STEMI patients treated with primary percutaneous coronary intervention (PPCI) from a historical (n=1155, 2002-2007) and contemporary (n=698, 2014-2022) cohort. Patients were grouped in tertiles according to leukocyte counts on day 3 after MI, as a surrogate parameter for delayed resolution of inflammation. In the historical cohort Serial single-photon emission computerized tomography imaging was available on admission and 7 to 14 days. Patients with elevated leukocyte counts after 72 h (T3 group) showed greatest area at risk (AAR) before PPCI (T1, AAR (median): 20.0% (IQR 11.0–36.0%); T2, AAR (median): 25.0% (IQR 14.0–40.0%), T3, AAR (median): 27.4% (IQR, 15.0–51.0%) and final infarct size (FIS) after 7 to 14 days after MI (T1, FIS (median): 7.0% (IQR 1.0–17.0%); T2, FIS (median): 12.0% (IQR 3.0–24.7%); T3, FIS (median): 13.0% (IQR 5.0–30.0%)) of the left ventricle. In line with these scintigraphic findings, peak creatine kinase myocardial band (CK-MB) values, as an enzymatic estimate of the infarct size, were also highest in T3. Additionally left ventricular ejection fraction (LV-EF) was lowest in the T3. At one year, 8 patients in T1, 7 patients in T2, and 22 patients in T3 had died (Kaplan–Meier estimates of 1-year mortality: 2.6%, 2.3%, and 7.3%, respectively (log-rank test: T1 vs. T3: p=0.01; T2 vs. T3: p=0.03). In the contemporary cohort we also found that patients with elevated leukocyte counts after 72 h (T3 group) showed greatest enzymatic infarct size, estimated by peak CK-MB values and reduced LV-EF. At one year, 6 patients in T1, 13 patients in T2 and 25 patients in T3 had died (Kaplan–Meier estimates of 1-year mortality: 3.8%, 8.3%, and 15.9%, respectively (log-rank test: T1 vs. T3: p<0.005, T2 vs. T3: p=0.004).
Conclusion: Delayed resolution of inflammation following MI, is associated with poorer outcomes at one year in STEMI patients.
- Graesser, Christian ( German Heart Centre Munich , Munich , Germany )
- Schunkert, Heribert ( German Heart Center , Munich , Germany )
- Ndrepepa, Gjin ( Deutsches Herzzentrum , Munich , Germany )
- Kastrati, Adnan ( Deutsches Herzzentrum , Munich , Germany )
- Kessler, Thorsten ( GERMAN HEART CENTRE MUNICH , Munich , Germany )
- Sager, Hendrik ( German Heart Center Munich , Munich , Germany )
- Krefting, Johannes ( German Heart Centre Munich , Munich , Germany )
- Voll, Felix ( German Heart Centre Munich , Munich , Germany )
- Trenkwalder, Teresa ( German Heart Centre Munich , Munich , Germany )
- Kufner, Sebastian ( Deutsches Herzzentrum Munich , Munich , Germany )
- Xhepa, Erion ( Deutsches Herzzentrum Munich , Munchen , Germany )
- Joner, Michael ( Deutsches Herzzentrum Muenchen , Munich , Germany )
- Cassese, Salvatore ( German Heart Centre Munich , Munich , Germany )
- Von Scheidt, Moritz ( DEUTSCHES HERZZENTRUM MUNICH , Munich , Germany )
Author Disclosures:
Christian Graesser: DO NOT have relevant financial relationships
| Heribert Schunkert: DO have relevant financial relationships
;
Consultant:Astra Zeneca:Active (exists now)
; Speaker:AMARIN:Active (exists now)
; Speaker:Sciarc:Active (exists now)
; Speaker:Bristol-Myers Squibb:Active (exists now)
; Speaker:Synlab:Active (exists now)
; Speaker:Sanofi-Aventis:Active (exists now)
; Speaker:Servier:Active (exists now)
; Speaker:Novartis:Active (exists now)
; Speaker:Bayer Vital:Active (exists now)
; Speaker:AstraZeneca:Active (exists now)
; Consultant:Servier:Active (exists now)
; Consultant:Daiichi-Sankyo:Active (exists now)
; Consultant:Boehringer Ingelheim:Active (exists now)
; Consultant:AMGEN:Active (exists now)
| Gjin Ndrepepa: DO NOT have relevant financial relationships
| Adnan Kastrati: DO NOT have relevant financial relationships
| Thorsten Kessler: DO NOT have relevant financial relationships
| Hendrik Sager: DO NOT have relevant financial relationships
| Johannes Krefting: DO NOT have relevant financial relationships
| Felix Voll: No Answer
| Teresa Trenkwalder: No Answer
| Sebastian Kufner: DO have relevant financial relationships
;
Speaker:BMS:Past (completed)
; Speaker:Abbott:Past (completed)
; Speaker:Translumina:Past (completed)
; Speaker:Boeringer Inglheim:Past (completed)
; Speaker:Astra Zeneca:Past (completed)
| Erion Xhepa: DO NOT have relevant financial relationships
| Michael Joner: DO have relevant financial relationships
;
Speaker:Abbott:Past (completed)
; Consultant:Veryan:Active (exists now)
; Consultant:TriCares:Active (exists now)
; Consultant:Shockwave:Active (exists now)
; Speaker:Shockwave:Past (completed)
; Speaker:ReCor:Past (completed)
; Speaker:Medtronic:Past (completed)
; Speaker:Edwards:Past (completed)
; Consultant:Edwards:Active (exists now)
; Consultant:Cardiac Dimensions:Active (exists now)
; Consultant:Boston Scientific:Active (exists now)
; Consultant:Biotronik:Active (exists now)
; Speaker:Biotronik:Past (completed)
; Speaker:AstraZeneca:Past (completed)
; Consultant:Alchimedics:Past (completed)
| Salvatore Cassese: No Answer
| Moritz Von Scheidt: DO NOT have relevant financial relationships
Meeting Info:
Session Info:
More abstracts on this topic:
Aging Heart Failure with Preserved Ejection Fraction is Mediated by Noncoding RNAs
Chakraborty Sankalpa, Dickerson Bryce, Bounds Curren, Lemus Sophia, Hickman Caleb, Rajagopalan Viswanathan
Aging-Associated Protein Medin Induces Human Coronary Artery Endothelial Proinflammatory and Prothrombotic ActivationKaramanova Nina, Morrow Kaleb, Maerivoet Alana, Madine Jillian, Li Ming, Migrino Raymond
More abstracts from these authors:
Duration of Antiplatelet Therapy and Risk of MACE in Patients With Coronary In-Stent Restenosis Treated With Second-Generation Drug-Eluting Stents or Drug-Coated Balloons
Krefting Johannes, Ramirez Santizo Daniela, Graesser Christian, Kruger Nils, Voll Felix, Von Scheidt Moritz, Kastrati Adnan, Schunkert Heribert, Kufner Sebastian
Outcomes of Drug-Coated Balloons versus Second-Generation Drug-Eluting Stents in In-Stent Restenosis: A Real-World PerspectiveKrefting Johannes, Kastrati Adnan, Schunkert Heribert, Von Scheidt Moritz, Wiebe Jens, Kruger Nils, Graesser Christian, Voll Felix, Cassese Salvatore, Sager Hendrik, Kessler Thorsten, Trenkwalder Teresa, Giacoppo Daniele
You have to be authorized to contact abstract author. Please, Login
Not Available