Final ID: Mo3153
Characterization of Novel Cardiovascular Medication Use by Clinical Specialty After Admission for Heart Failure or Coronary Artery Disease
Abstract Body (Do not enter title and authors here): Background:
Angiotensin receptor-neprilysin inhibitors (ARNI), sodium-glucose cotransporter-2 inhibitors (SGLT2i), and glucagon-like peptide-1 receptor agonists (GLP-1 RA) have well-established benefit for patients with heart failure (HF) or coronary artery disease with type 2 diabetes (CAD+T2D), but use remains low. We aimed to characterize post-hospitalization use of these novel medications by provider specialty in the Veterans Health Administration (VA).
Methods:
Using VA health record and administrative data, two patient cohorts were retrospectively identified with hospitalization from 2017-2023 for either HF or CAD+T2D. Provider-level encounter data and outpatient prescriptions within 6 months of discharge were assessed for ARNI and SGLT2i for HF and SGTL2i or GLP-1 RA for CAD+T2D among primary care, cardiology, endocrinology, and nephrology providers. Medication utilization was counted equally for providers seeing the same patient, regardless of which provider initiated the prescription. Descriptive statistics were used to characterize frequency and proportions of novel medication use by specialty in 4 categories with respect to hospital discharge: 1) only before, 2) continued, 3) new start, or 4) untreated.
Results:
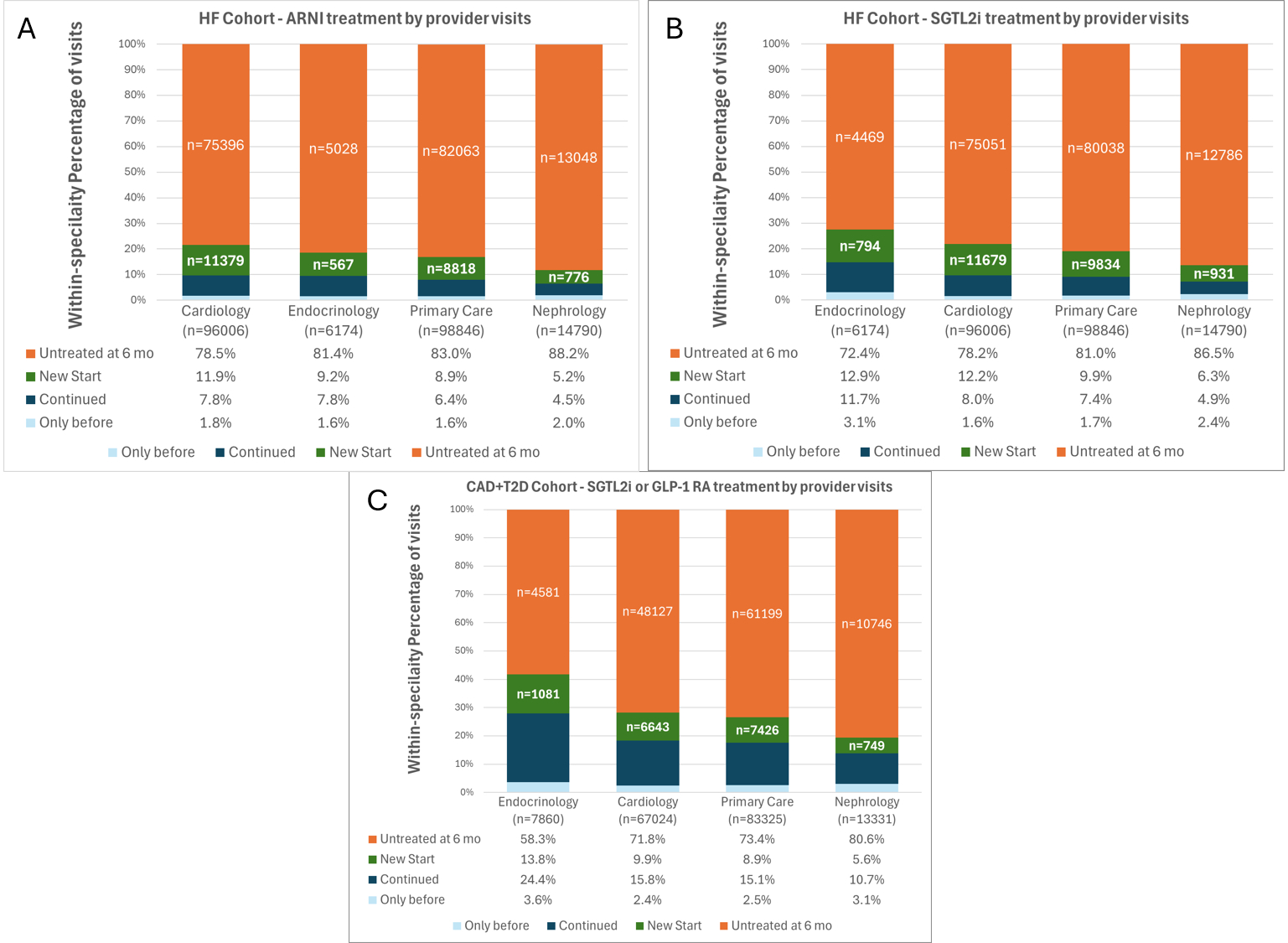
There were 215,816 patient-provider encounters in the HF cohort and 171,540 encounters in the CAD+T2D cohort. Cardiology providers had the highest rate (11.9%) and largest number (n=11,397) of new starts for ARNI. For SGLT2i for HF, endocrinology had the highest rate (12.9%) but the smallest number (n=794) of new starts. For SGTL2i or GLP-1 RA for CAD+T2D, endocrinology had the highest rate (13.8%), but primary care had the highest number (n=7,426) of new starts. In total, 10% of visits had a new start while >70% of patients were untreated with novel medication classes.
Conclusion:
Most post-hospitalization care for HF and CAD+T2D was provided by primary care and cardiology. Cardiologists and endocrinologists were most likely to use novel cardiovascular medications, but endocrinologists accounted for a small proportion of total HF and CAD care. Future work should focus on implementation strategies to address the large opportunity for improvement in guideline-concordant care across all specialties.
Angiotensin receptor-neprilysin inhibitors (ARNI), sodium-glucose cotransporter-2 inhibitors (SGLT2i), and glucagon-like peptide-1 receptor agonists (GLP-1 RA) have well-established benefit for patients with heart failure (HF) or coronary artery disease with type 2 diabetes (CAD+T2D), but use remains low. We aimed to characterize post-hospitalization use of these novel medications by provider specialty in the Veterans Health Administration (VA).
Methods:
Using VA health record and administrative data, two patient cohorts were retrospectively identified with hospitalization from 2017-2023 for either HF or CAD+T2D. Provider-level encounter data and outpatient prescriptions within 6 months of discharge were assessed for ARNI and SGLT2i for HF and SGTL2i or GLP-1 RA for CAD+T2D among primary care, cardiology, endocrinology, and nephrology providers. Medication utilization was counted equally for providers seeing the same patient, regardless of which provider initiated the prescription. Descriptive statistics were used to characterize frequency and proportions of novel medication use by specialty in 4 categories with respect to hospital discharge: 1) only before, 2) continued, 3) new start, or 4) untreated.
Results:
There were 215,816 patient-provider encounters in the HF cohort and 171,540 encounters in the CAD+T2D cohort. Cardiology providers had the highest rate (11.9%) and largest number (n=11,397) of new starts for ARNI. For SGLT2i for HF, endocrinology had the highest rate (12.9%) but the smallest number (n=794) of new starts. For SGTL2i or GLP-1 RA for CAD+T2D, endocrinology had the highest rate (13.8%), but primary care had the highest number (n=7,426) of new starts. In total, 10% of visits had a new start while >70% of patients were untreated with novel medication classes.
Conclusion:
Most post-hospitalization care for HF and CAD+T2D was provided by primary care and cardiology. Cardiologists and endocrinologists were most likely to use novel cardiovascular medications, but endocrinologists accounted for a small proportion of total HF and CAD care. Future work should focus on implementation strategies to address the large opportunity for improvement in guideline-concordant care across all specialties.
More abstracts on this topic:
6-Nitrodopamine potentiates the positive chronotopic and inotropic effect induced by noradrenaline in the rat isolated heart
Lima Antonio, Sobanski Joao Fernando, Antunes Edson, De Nucci Gilberto
A Health Coach-Based Multi-Level Personalized Strategy Lowers LDL-Cholesterol and Enhances Lipid Control in Veterans with Atherosclerotic Cardiovascular Disease – The VA Lipid Optimization Reimagined Quality Improvement Project at VA New York Harbor Healthcare SystemChen Tina, Ingerman Diana, Haley Leah, Salovaara Priscilla, Nicholson Andrew, Illenberger Nicholas, Natarajan Sundar