Final ID: Su3177
Commercial Pricing of Percutaneous Coronary Intervention in The United States
Abstract Body (Do not enter title and authors here): Background:
The 2021 Price Transparency Final Rule required hospitals to publicly disclose commercial prices for all medical services. Using data made available by this legislation, we investigated variation in inpatient prices for percutaneous coronary intervention (PCI).
Hypothesis:
We hypothesized that there would be substantial differences in commercial prices between and within hospitals and that this variation would be associated with factors such as market competitiveness rather than patient outcomes.
Methods:
PCI hospitalization prices (MS-DRG 247-251) were obtained from Turquoise Health and linked to hospital characteristics. The association between price and hospital factors such as the Herfindahl–Hirschman index (HHI) for market competitiveness was evaluated using linear models. We also included hospital acute myocardial infarction (AMI) specific mortality and readmission rates made publicly available by Medicare.
Results:
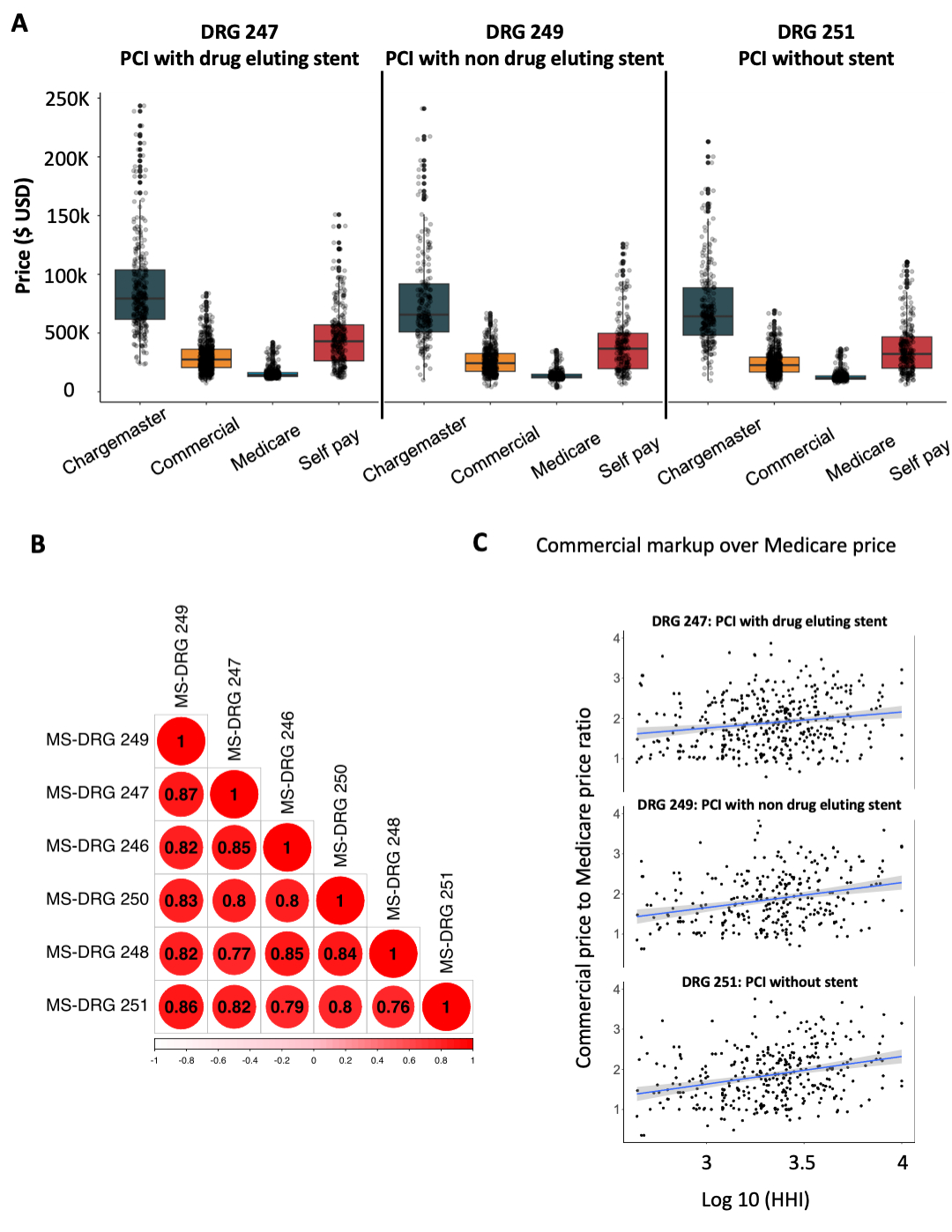
Median commercial prices (N = 523 hospitals) were 1.7-1.9x higher than Medicare rates (Fig 1A). Self-pay prices were 2.4-3.0x higher. There was strong price correlation across DRG codes (Fig 1B). Across hospitals, the 90th percentile price was >2.5x the 10th percentile price. Within hospitals, the 90th percentile price was 1.7-2.1x the 10th percentile price. Prices varied greatly by region, with the Pacific being the most expensive and Midwest the least. For PCI with drug-eluting stents (DRG 246-247), teaching hospitals had higher prices than non-teaching hospitals (95% CI: +$4,000-5,000) whereas investor-owned hospitals had lower prices (95% CI: -$6,000-$9,000). Higher prices were not linked to hospital readmission and mortality statistics for AMI. On a system level, less competitive markets had significantly higher markups over Medicare rates (Fig 1C).
Conclusion:
Prices for PCI hospitalization vary significantly within and between hospitals and appear associated with hospital and system-level characteristics.
The 2021 Price Transparency Final Rule required hospitals to publicly disclose commercial prices for all medical services. Using data made available by this legislation, we investigated variation in inpatient prices for percutaneous coronary intervention (PCI).
Hypothesis:
We hypothesized that there would be substantial differences in commercial prices between and within hospitals and that this variation would be associated with factors such as market competitiveness rather than patient outcomes.
Methods:
PCI hospitalization prices (MS-DRG 247-251) were obtained from Turquoise Health and linked to hospital characteristics. The association between price and hospital factors such as the Herfindahl–Hirschman index (HHI) for market competitiveness was evaluated using linear models. We also included hospital acute myocardial infarction (AMI) specific mortality and readmission rates made publicly available by Medicare.
Results:
Median commercial prices (N = 523 hospitals) were 1.7-1.9x higher than Medicare rates (Fig 1A). Self-pay prices were 2.4-3.0x higher. There was strong price correlation across DRG codes (Fig 1B). Across hospitals, the 90th percentile price was >2.5x the 10th percentile price. Within hospitals, the 90th percentile price was 1.7-2.1x the 10th percentile price. Prices varied greatly by region, with the Pacific being the most expensive and Midwest the least. For PCI with drug-eluting stents (DRG 246-247), teaching hospitals had higher prices than non-teaching hospitals (95% CI: +$4,000-5,000) whereas investor-owned hospitals had lower prices (95% CI: -$6,000-$9,000). Higher prices were not linked to hospital readmission and mortality statistics for AMI. On a system level, less competitive markets had significantly higher markups over Medicare rates (Fig 1C).
Conclusion:
Prices for PCI hospitalization vary significantly within and between hospitals and appear associated with hospital and system-level characteristics.
More abstracts on this topic:
Assessing the Efficacy of Preventive Percutaneous Coronary Intervention vs Optimal Medical Therapy for the Treatment of Vulnerable Plaque: A Meta-analysis
Mootz Nicholas, Rojulpote Chaitanya, Verma Divya, Harjai Kishore, Lin Chien-jung
Abbreviated Ticagrelor-Based Dual Antiplatelet Therapy in Acute Coronary Syndrome: A Systematic Review and Meta-AnalysisHarmouch Wissam, Elbadawi Ayman, Thakker Ravi, Khalid Umair, Khalife Wissam, Kleiman Neal, Rangasetty Umamahesh, Kayani Waleed, Jneid Hani, Al Hemyari Bashar