Final ID: Sa1113
Ultrasound-Targeted Microbubble Cavitation For The Treatment Of Myocardial Microvascular Obstruction: A Porcine Study
Abstract Body (Do not enter title and authors here): Introduction
In 2019, 17.9 million people died from cardiovascular disease, 85% of which were due to acute myocardial infarction (AMI). Post-AMI congestive heart failure is increasing due to microvascular obstruction (MVO). MVO is the blockage of the microcirculation by atherothrombotic debris and tends to occur after coronary stenting for AMI. Current therapeutic strategies for MVO are not consistently effective.
Aim
Our goal is to develop ultrasound (US)-targeted microbubble cavitation (UTMC) as a potential treatment for MVO.
Methods
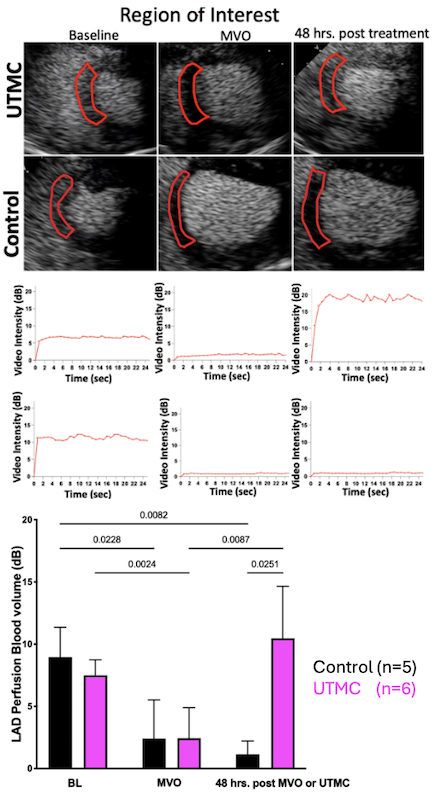
Initially, we demonstrated the efficacy of UTMC in a rat hindlimb model of MVO. Given these promising findings, in the current work, we expanded our investigation to a clinically relevant porcine model of myocardial MVO. On day 1, MVO was created in the left anterior descending (LAD) microcirculation and confirmed by myocardial contrast echocardiography (MCE). The MVO in the LAD bed was then treated with UTMC therapy during concurrent infusion of Definity® contrast agent. The therapeutic ultrasound (1.3 MHz center frequency, 1.3 MPa peak negative pressure, 1 ms pulse duration) was delivered with Philips EpiQ (with S5-1 probe). Cardiac MRI was obtained at 36 hours to measure infarct size and area of MVO. At 48 hours post UTMC therapy, MCE was repeated, and the animals were euthanized. Hearts were stained with Evans Blue/ TTC dyes and sectioned for analysis of infarct size. A total of 11 pigs, 5 Control (MVO, no treatment) and 6 UTMC (MVO, UTMC treatment) were done.
Results
LAD angiographic flow was improved at 48 hours post UTMC treatment in comparison to control. MCE imaging revealed that the UTMC treatment significantly improved LV systolic performance, and LAD blood volume (Figure 1), as compared to control. MRI clips showed that UTMC ameliorated MVO and left ventricular (LV) segmental wall motion and ejection fraction (EF) also improved after UTMC treatment versus control. Infarct size was reduced as shown by both Evans Blue/TTC staining and MRI.
Conclusions
Taken together, we demonstrated that UTMC significantly reduced infarct size, enhanced LAD microvascular perfusion and improved LV systolic performance, and should enable clinical translation of this promising therapy.
In 2019, 17.9 million people died from cardiovascular disease, 85% of which were due to acute myocardial infarction (AMI). Post-AMI congestive heart failure is increasing due to microvascular obstruction (MVO). MVO is the blockage of the microcirculation by atherothrombotic debris and tends to occur after coronary stenting for AMI. Current therapeutic strategies for MVO are not consistently effective.
Aim
Our goal is to develop ultrasound (US)-targeted microbubble cavitation (UTMC) as a potential treatment for MVO.
Methods
Initially, we demonstrated the efficacy of UTMC in a rat hindlimb model of MVO. Given these promising findings, in the current work, we expanded our investigation to a clinically relevant porcine model of myocardial MVO. On day 1, MVO was created in the left anterior descending (LAD) microcirculation and confirmed by myocardial contrast echocardiography (MCE). The MVO in the LAD bed was then treated with UTMC therapy during concurrent infusion of Definity® contrast agent. The therapeutic ultrasound (1.3 MHz center frequency, 1.3 MPa peak negative pressure, 1 ms pulse duration) was delivered with Philips EpiQ (with S5-1 probe). Cardiac MRI was obtained at 36 hours to measure infarct size and area of MVO. At 48 hours post UTMC therapy, MCE was repeated, and the animals were euthanized. Hearts were stained with Evans Blue/ TTC dyes and sectioned for analysis of infarct size. A total of 11 pigs, 5 Control (MVO, no treatment) and 6 UTMC (MVO, UTMC treatment) were done.
Results
LAD angiographic flow was improved at 48 hours post UTMC treatment in comparison to control. MCE imaging revealed that the UTMC treatment significantly improved LV systolic performance, and LAD blood volume (Figure 1), as compared to control. MRI clips showed that UTMC ameliorated MVO and left ventricular (LV) segmental wall motion and ejection fraction (EF) also improved after UTMC treatment versus control. Infarct size was reduced as shown by both Evans Blue/TTC staining and MRI.
Conclusions
Taken together, we demonstrated that UTMC significantly reduced infarct size, enhanced LAD microvascular perfusion and improved LV systolic performance, and should enable clinical translation of this promising therapy.
More abstracts on this topic:
Apabetalone: evaluating cardiovascular and safety outcomes in meta-analysis
Tanriverdi Lokman Hekim, Dogan Muhammed Melih, Bytyci Ibadete, Penson Peter, Toth Peter, Banach Maciej
Carotid Plaque Microplastics are Associated with Clinical Symptoms and Mesenchymal Stem Cell-Macrophage Immunomodulatory EffectsClark Ross, Campen Matthew, Massie Pierce, Garcia Marcus, Decker Aerlin, Liu Rui, Mazloumibakhshayesh Milad, Kulkarni Deepali, Rana Ali, Pace Carolyn