Final ID: Sa4007
Optimal Timing for Coronary Artery Bypass Grafting in NSTEMI Patients: A Retrospective Cohort Analysis of In-Hospital Mortality and Stroke Prevalence Over 2017 to 2021
Abstract Body (Do not enter title and authors here):
Background
Recent studies have suggested performing coronary artery bypass grafting (CABG) within 24 hours of acute myocardial infarction increases mortality risk. However, the ideal timing after the first day remains unclear. This study aims to suggest an optimal timing of CABG in NSTEMI patients using the large National Inpatient Sample (NIS) database over a 5-year period.
Methods
This retrospective cohort study analyzed survey-weighted NIS data over 2017-2021, including adult-age admissions with NSTEMI as the principal diagnosis who underwent CABG without prior transfer from another hospital. Patients were categorized into eight groups based on days from admission to CABG (0, 1, 2, 3, 4, 5, 6, and ≥7 days). Baseline characteristics were compared across groups. Multivariate regression analysis adjusted for multiple confounders to assess the association between Time-to-CABG and in-hospital mortality and stroke prevalence.
Results
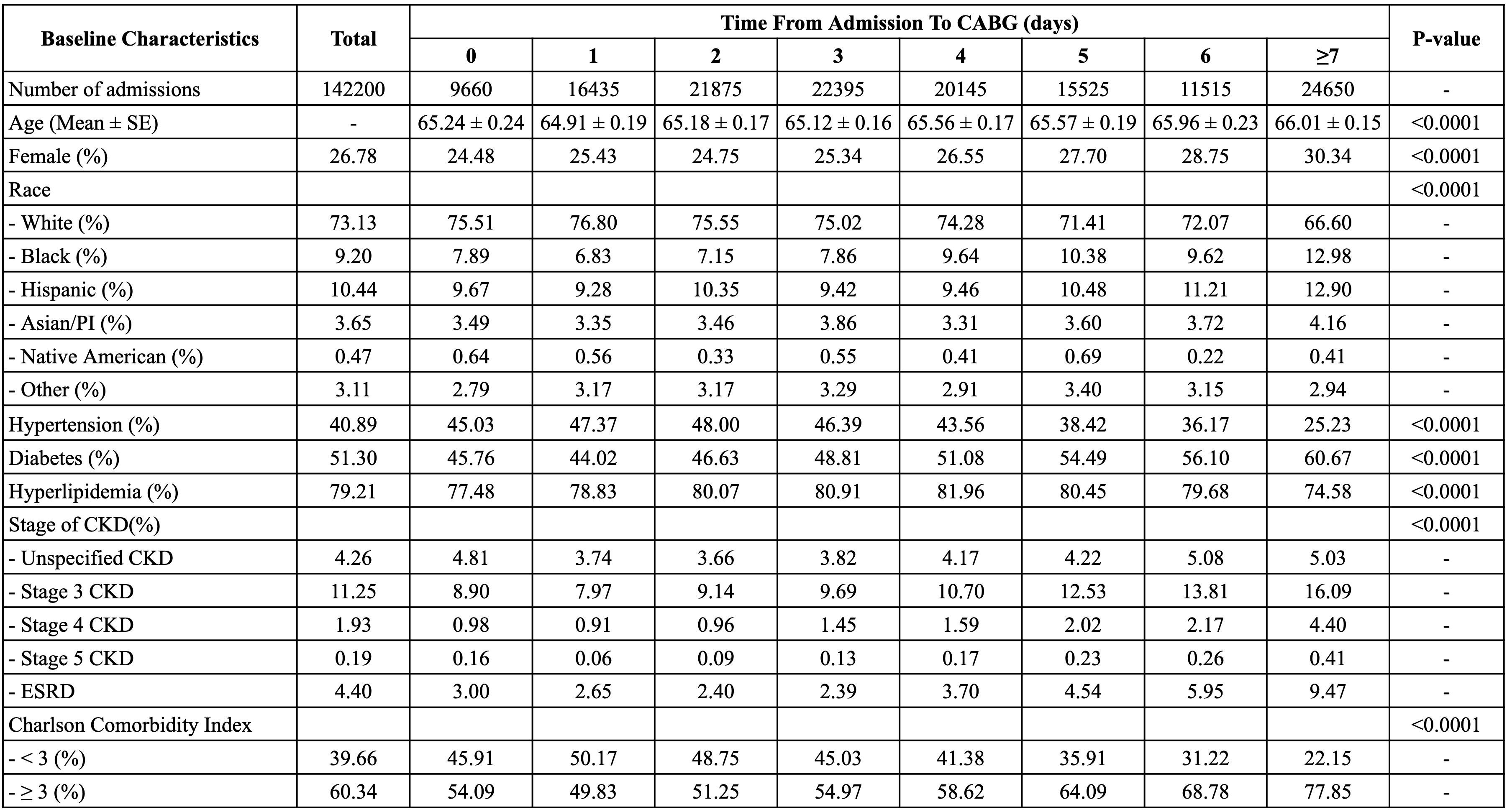
Table 1 presents the baseline characteristics across the eight groups, encompassing 142,200 included admissions (mean age 65.24 years; 26.78% female).
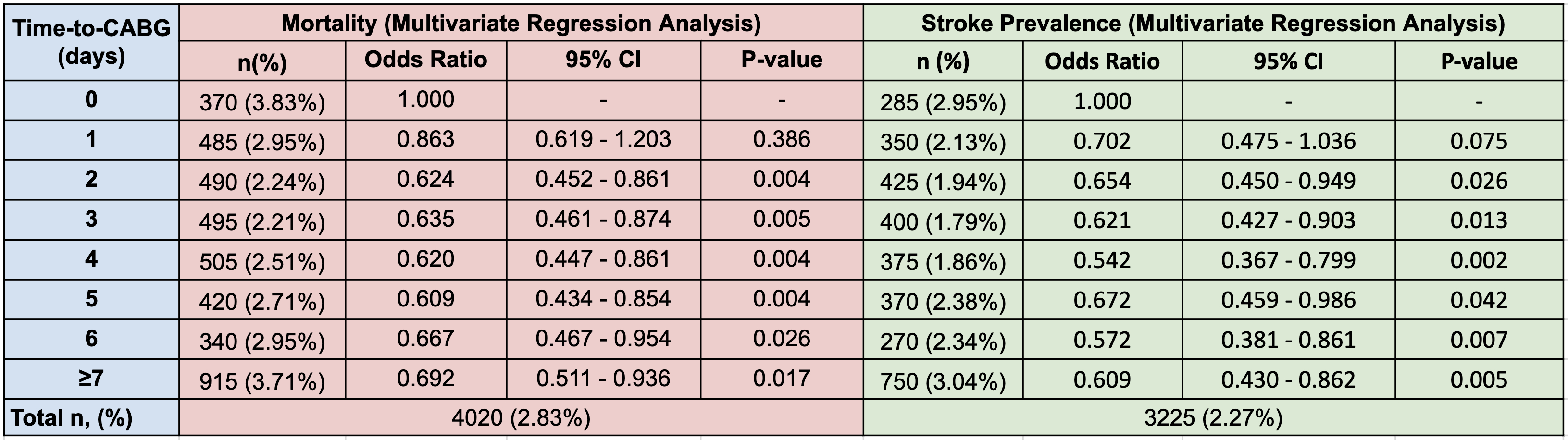
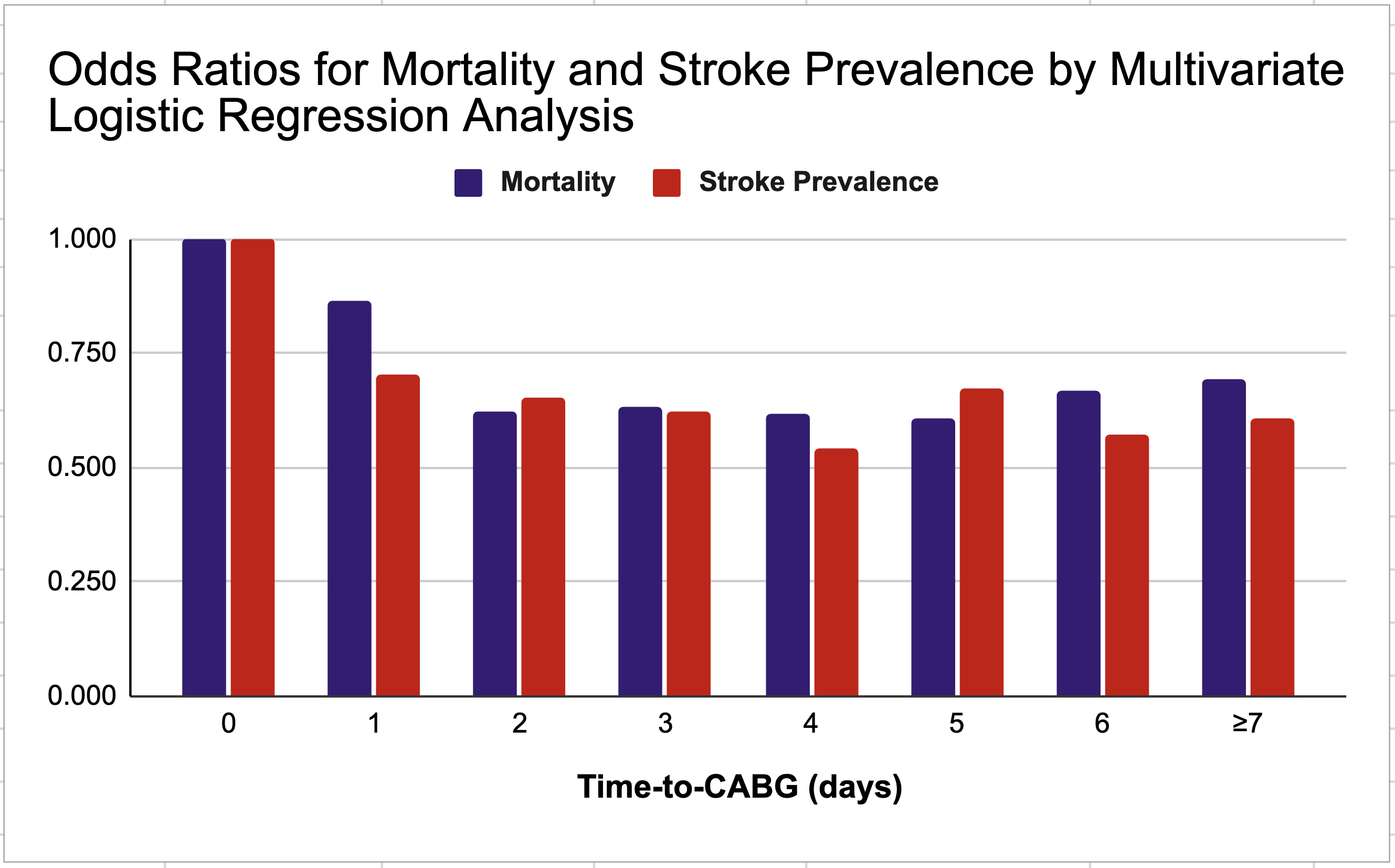
In-Hospital Mortality: The adjusted odds ratios (OR) were less than one for groups 1 through 7 compared to group 0, indicating that immediate CABG (day 0) is associated with higher mortality risk. While the reduced odds in the day 1 group were not statistically significant, substantial and statistically significant reductions in mortality were observed between days 2 and 5 (OR: 0.624 - 0.609; p<0.05). After day 5, the OR for mortality trended up, reaching 0.667 (p<0.05) on day 6 and 0.692 (p<0.05) for surgeries performed on day 7 or later.
Stroke Prevalence: The adjusted ORs for stroke prevalence were significantly lower for groups 1 through 7 compared to the CABG within 24-hour group (all p-values <0.05). The lowest ORs were observed between days 2 and 4 (OR: 0.654 and 0.542, p<0.05, respectively). After day 4, the ORs increased, reaching 0.672 (p<0.05) for surgeries performed on day 5 and 0.609 (p<0.05) on day 7 and beyond.
Conclusion
The mortality risk in NSTEMI patients remained higher if CABG was performed in the first 48 hours of admission (end of day 1) compared to later. This risk also increased if CABG was done after day 5. Combined with the possible risk of stroke being increased from day 5, we suggest the optimal time-to-CABG is between admission day 2 and day 4 in NSTEMI patients. Future prospective studies are warranted to confirm these findings and guide clinical practice.
Background
Recent studies have suggested performing coronary artery bypass grafting (CABG) within 24 hours of acute myocardial infarction increases mortality risk. However, the ideal timing after the first day remains unclear. This study aims to suggest an optimal timing of CABG in NSTEMI patients using the large National Inpatient Sample (NIS) database over a 5-year period.
Methods
This retrospective cohort study analyzed survey-weighted NIS data over 2017-2021, including adult-age admissions with NSTEMI as the principal diagnosis who underwent CABG without prior transfer from another hospital. Patients were categorized into eight groups based on days from admission to CABG (0, 1, 2, 3, 4, 5, 6, and ≥7 days). Baseline characteristics were compared across groups. Multivariate regression analysis adjusted for multiple confounders to assess the association between Time-to-CABG and in-hospital mortality and stroke prevalence.
Results
Table 1 presents the baseline characteristics across the eight groups, encompassing 142,200 included admissions (mean age 65.24 years; 26.78% female).
In-Hospital Mortality: The adjusted odds ratios (OR) were less than one for groups 1 through 7 compared to group 0, indicating that immediate CABG (day 0) is associated with higher mortality risk. While the reduced odds in the day 1 group were not statistically significant, substantial and statistically significant reductions in mortality were observed between days 2 and 5 (OR: 0.624 - 0.609; p<0.05). After day 5, the OR for mortality trended up, reaching 0.667 (p<0.05) on day 6 and 0.692 (p<0.05) for surgeries performed on day 7 or later.
Stroke Prevalence: The adjusted ORs for stroke prevalence were significantly lower for groups 1 through 7 compared to the CABG within 24-hour group (all p-values <0.05). The lowest ORs were observed between days 2 and 4 (OR: 0.654 and 0.542, p<0.05, respectively). After day 4, the ORs increased, reaching 0.672 (p<0.05) for surgeries performed on day 5 and 0.609 (p<0.05) on day 7 and beyond.
Conclusion
The mortality risk in NSTEMI patients remained higher if CABG was performed in the first 48 hours of admission (end of day 1) compared to later. This risk also increased if CABG was done after day 5. Combined with the possible risk of stroke being increased from day 5, we suggest the optimal time-to-CABG is between admission day 2 and day 4 in NSTEMI patients. Future prospective studies are warranted to confirm these findings and guide clinical practice.
More abstracts on this topic:
AI and Quantum Sensors:
Realization of a Safe and Effective Unshielded Bedside Magnetocardiogram to Detect Ischemia in the Emergency Room
Realization of a Safe and Effective Unshielded Bedside Magnetocardiogram to Detect Ischemia in the Emergency Room
Iwata Geoffrey, Aschbacher Kirstin, John Sajiny, Tam Simon, Au-yeung Kit Yee, Contreras Johanna, Bhatt Deepak, Bander Jeffrey
A Bridge from Sweet to Sour: A Case of Recurrent Myocardial Stunning in Diabetic KetoacidosisSatish Vikyath, Pargaonkar Sumant, Slipczuk Leandro, Schenone Aldo, Maliha Maisha, Chi Kuan Yu, Sunil Kumar Sriram, Borkowski Pawel, Vyas Rhea, Rodriguez Szaszdi David Jose Javier, Kharawala Amrin, Seo Jiyoung