Final ID: MDP559
Inter-hospital Transfer for Cardiogenic Shock patients: Contemporary Strategies and Outcomes
Abstract Body (Do not enter title and authors here): Background: Cardiogenic shock (CS) is often managed with strategies that require inter-hospital transfers. The contemporary practice patterns and outcomes of transferred CS are unknown.
Methods: Patients with CS were identified using ICD-10 codes in Medicare claims from 2016-2021. We used a logistic regression model to assess the association of hospital transfer with mortality. We conducted a sensitivity analysis examining the association of early transfer (≤ 24 hours) versus later transfer (>24 hours) and mortality.
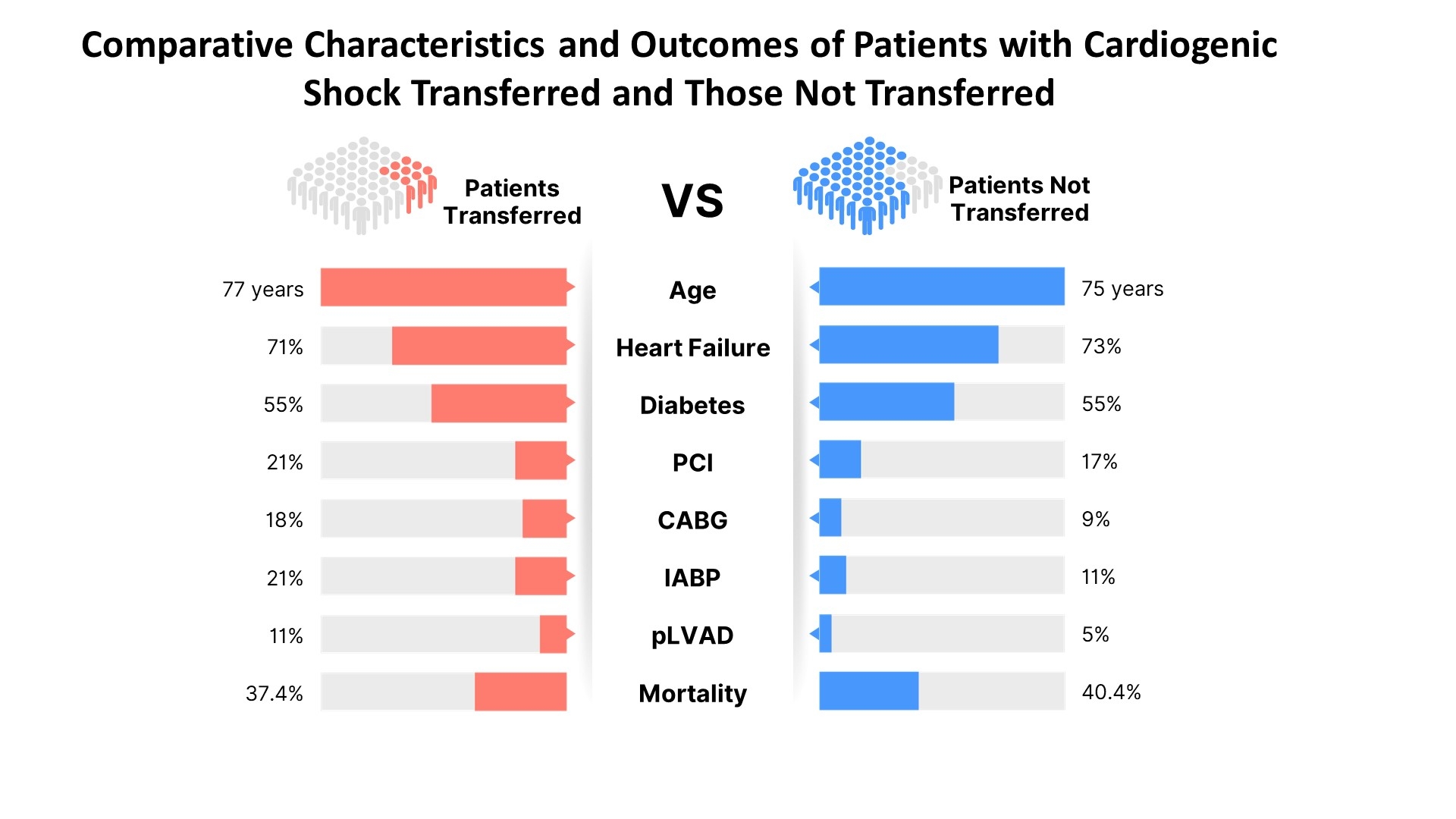
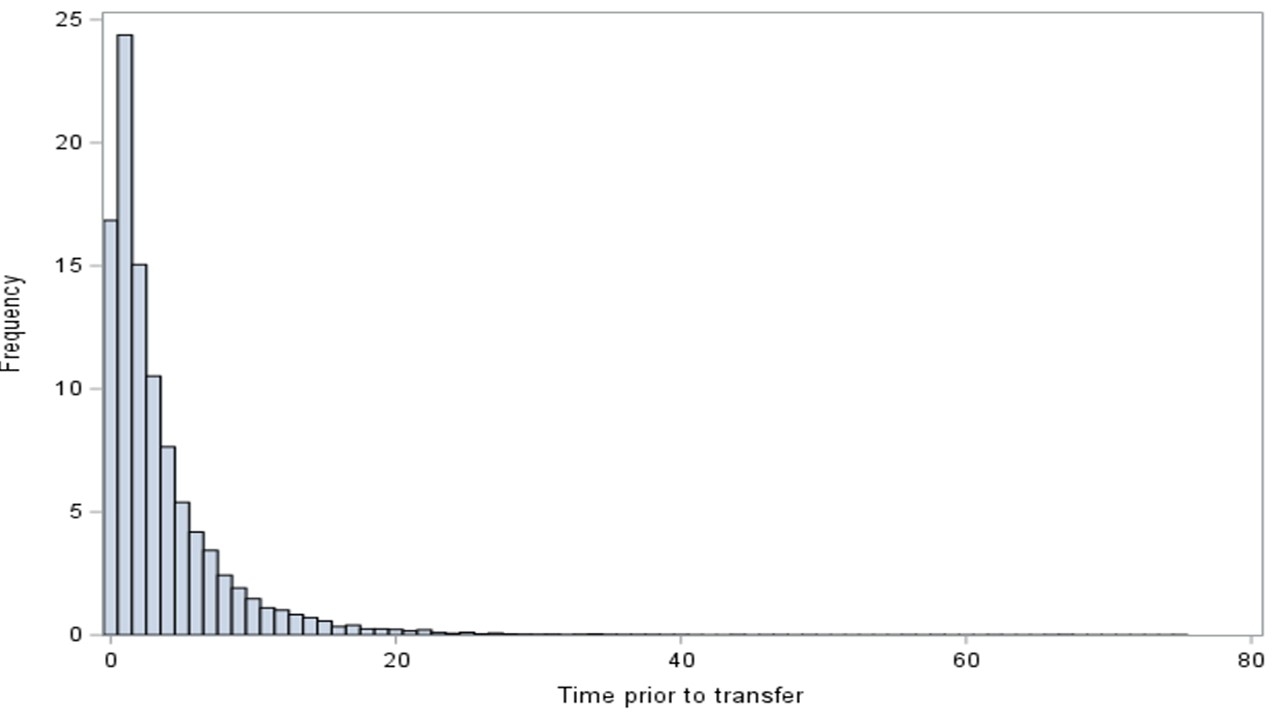
Results: We identified 260,092 patients with CS; of which 9.7% required inter-hospital transfer. Mean time to transfer was 3.5 days (Figure). Transferring hospitals were smaller (229 versus 396 beds), less likely teaching hospitals (43% versus 70%), and more likely rural (7% versus 0.4%). Compared with patients with CS that were not transferred, transferred patients were were older (77 versus 75 years) and had comparable co-morbidity burdens (heart failure 71% versus 73%, diabetes 55% versus 55%). Transferred patients were more likely to receive PCI (21% versus 17%), CABG (18% versus 9%), and MCS, including intra-aortic balloon pumps (21% versus 11%) and percutaneous left ventricular assist devices (11% versus 5%). Transferred patients had longer hospital length of stay (17.8 versus 9.8 days) and ICU length of stay (9.7 days versus 5.6 days). Observed mortality for transferred versus not transferred patients with CS was 37.4% and 40.4% respectively. In addition, transferred patients were associated with a lower mortality (adjusted OR 0.78; 95% CI: 0.76 – 0.81). Early transfer was associated with a slightly lower mortality compared with later transfer (36% vs 38%; p < 0.01).
Conclusions: Nearly 10% of older patients with CS are transferred to another hospital. Transferred patients were more likely to be treated with revascularization and MCS. Transfer of patients with CS was associated with a lower mortality, especially if the transfer is early within the first 24 hours.
Methods: Patients with CS were identified using ICD-10 codes in Medicare claims from 2016-2021. We used a logistic regression model to assess the association of hospital transfer with mortality. We conducted a sensitivity analysis examining the association of early transfer (≤ 24 hours) versus later transfer (>24 hours) and mortality.
Results: We identified 260,092 patients with CS; of which 9.7% required inter-hospital transfer. Mean time to transfer was 3.5 days (Figure). Transferring hospitals were smaller (229 versus 396 beds), less likely teaching hospitals (43% versus 70%), and more likely rural (7% versus 0.4%). Compared with patients with CS that were not transferred, transferred patients were were older (77 versus 75 years) and had comparable co-morbidity burdens (heart failure 71% versus 73%, diabetes 55% versus 55%). Transferred patients were more likely to receive PCI (21% versus 17%), CABG (18% versus 9%), and MCS, including intra-aortic balloon pumps (21% versus 11%) and percutaneous left ventricular assist devices (11% versus 5%). Transferred patients had longer hospital length of stay (17.8 versus 9.8 days) and ICU length of stay (9.7 days versus 5.6 days). Observed mortality for transferred versus not transferred patients with CS was 37.4% and 40.4% respectively. In addition, transferred patients were associated with a lower mortality (adjusted OR 0.78; 95% CI: 0.76 – 0.81). Early transfer was associated with a slightly lower mortality compared with later transfer (36% vs 38%; p < 0.01).
Conclusions: Nearly 10% of older patients with CS are transferred to another hospital. Transferred patients were more likely to be treated with revascularization and MCS. Transfer of patients with CS was associated with a lower mortality, especially if the transfer is early within the first 24 hours.
More abstracts on this topic:
A Retrospective Analysis of Chronic Kidney Disease and Arrhythmias-Related Mortality Among Adults in the United States (1999-2020): Insights into Disparities by Gender, Race/Ethnicity, and Geography
Waseem Neha, Nouman Zainab, Chaudhry Sohaib Aftab Ahmad, Tariq Waleed, Khan Iftikhar, Shah Mazhar, Farooqi Hanzala Ahmed, Faiz Muneeb
Accelerometer-Measured Sedentary Behavior and Future Cardiovascular DiseaseAjufo Ezimamaka, Kany Shinwan, Ramo Joel, Churchill Timothy, Guseh James, Aragam Krishna, Ellinor Patrick, Khurshid Shaan