Final ID: MDP685
All-Cause Mortality and Cardiovascular Outcomes with Glucagon-Like Peptide-1 Receptor Agonists in People with Type 2 Diabetes and Systolic Heart Failure
Abstract Body (Do not enter title and authors here): Background
There is an increasing prevalence of type 2 diabetes (T2D) and systolic heart failure. Glucagon-like peptide-1 receptor agonists (GLP-1 RA) are becoming popular in the management of T2D. Previous studies have demonstrated that GLP-1 RAs reduce major adverse cardiovascular events (MACE) in T2D patients compared to placebo. However, the impact of GLP-1 RAs on mortality and cardiovascular outcomes in patients with T2D and systolic heart failure remains uncertain.
Aim
This study examines the effects of GLP-1 RA on individuals with T2D and systolic heart failure, focusing on all-cause mortality, cardiovascular outcomes (including ischemic heart disease, acute myocardial infarction, heart failure exacerbations, stroke, peripheral vascular disease, chronic kidney disease), and all-cause hospitalization.
Methods
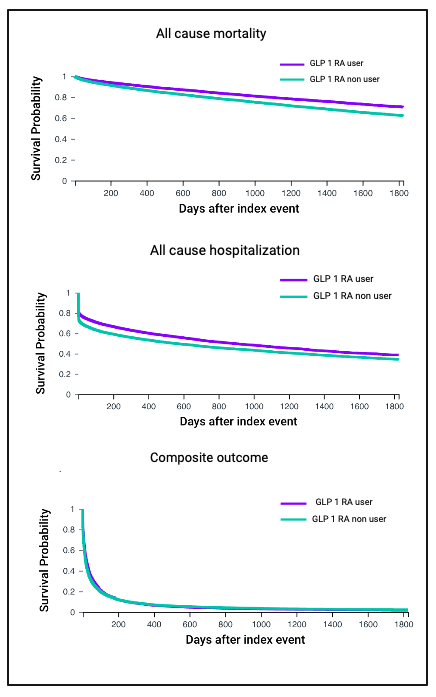
The TriNetX research database was utilized to identify patients aged 18 years and older with T2D and systolic heart failure. Patients were classified into two groups: GLP-1 RA users and non-users. Propensity score matching (1:1) was conducted based on demographics, body mass index, comorbidities, glycated hemoglobin levels, and medications, resulting in a matched cohort of 23,873 patients. Outcomes analyzed included all-cause mortality, cardiovascular outcomes and all cause hospitalization. Survival analysis was performed using TriNetX software, estimating the probability of outcomes over 5 years from the index event and generating hazard ratios (HR), log-rank tests, and Kaplan-Meier survival curves.
Results
The GLP-1 RA user group demonstrated a reduced hazard ratio (HR, 95% confidence interval) over 5 years compared with the control group for all-cause mortality (0.705, 0.675-0.736, P <0.001), composite of cardiovascular outcomes (0.94, 0.922-0.958, P<0.001), all cause hospitalization (0.809, 0.788-0.831, P <0.001) (Figure), acute myocardial infarction (0.822, 0.790-0.857, P <0.001), and heart failure exacerbation (0.962, 0.944-0.981, P <0.001). All other individual cardiovascular outcomes also showed significant risk reductions in favor of the GLP-1 RA cohort.
Conclusion
In patients with type 2 diabetes and systolic heart failure, GLP-1 RA therapy significantly reduces mortality and cardiovascular events over a 5-year period, independent of body weight.
There is an increasing prevalence of type 2 diabetes (T2D) and systolic heart failure. Glucagon-like peptide-1 receptor agonists (GLP-1 RA) are becoming popular in the management of T2D. Previous studies have demonstrated that GLP-1 RAs reduce major adverse cardiovascular events (MACE) in T2D patients compared to placebo. However, the impact of GLP-1 RAs on mortality and cardiovascular outcomes in patients with T2D and systolic heart failure remains uncertain.
Aim
This study examines the effects of GLP-1 RA on individuals with T2D and systolic heart failure, focusing on all-cause mortality, cardiovascular outcomes (including ischemic heart disease, acute myocardial infarction, heart failure exacerbations, stroke, peripheral vascular disease, chronic kidney disease), and all-cause hospitalization.
Methods
The TriNetX research database was utilized to identify patients aged 18 years and older with T2D and systolic heart failure. Patients were classified into two groups: GLP-1 RA users and non-users. Propensity score matching (1:1) was conducted based on demographics, body mass index, comorbidities, glycated hemoglobin levels, and medications, resulting in a matched cohort of 23,873 patients. Outcomes analyzed included all-cause mortality, cardiovascular outcomes and all cause hospitalization. Survival analysis was performed using TriNetX software, estimating the probability of outcomes over 5 years from the index event and generating hazard ratios (HR), log-rank tests, and Kaplan-Meier survival curves.
Results
The GLP-1 RA user group demonstrated a reduced hazard ratio (HR, 95% confidence interval) over 5 years compared with the control group for all-cause mortality (0.705, 0.675-0.736, P <0.001), composite of cardiovascular outcomes (0.94, 0.922-0.958, P<0.001), all cause hospitalization (0.809, 0.788-0.831, P <0.001) (Figure), acute myocardial infarction (0.822, 0.790-0.857, P <0.001), and heart failure exacerbation (0.962, 0.944-0.981, P <0.001). All other individual cardiovascular outcomes also showed significant risk reductions in favor of the GLP-1 RA cohort.
Conclusion
In patients with type 2 diabetes and systolic heart failure, GLP-1 RA therapy significantly reduces mortality and cardiovascular events over a 5-year period, independent of body weight.
More abstracts on this topic:
A Model-Sharing Approach for Quality Improvement of Diabetes and Cardiovascular Disease
Elligers Kyle, Pollner Meghan, Overton Katherine, Congdon Michelle, Greenway Stacey, Lambro Patricia, Sadiku Steven, Schechter Rona, Whelan John, Pressley Bianca, Sednew Renee, Duckett Sara
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responsesShao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng