Final ID: Su3110
GLP-1 Agonists are Associated with Fewer Unplanned Hospital Visits in Patients with Cardiovascular Disease and Comorbid Substance Use Disorder
Abstract Body (Do not enter title and authors here): Background:
Improved outcomes related to the use of glucagon-like peptide 1 (GLP-1) agonists in patients with cardiovascular disease (CVD) have been well documented. Small studies have shown benefits of GLP-1 agonists in reducing substance use in patients with substance use disorders (SUDs). In patients with CVD, co-occurring SUDs are known to worsen outcomes. The use of GLP-1 agonists to improve outcomes related to both CVD and SUD could improve healthcare disparities in this marginalized population.
Hypothesis:
The use of GLP-1 agonists in patients with CVD and SUD could improve outcomes related to both disease processes.
Aim:
Our aim is to describe clinical outcomes in patients with CVD and SUD who were prescribed GLP-1 agonists.
Methods:
This is a single-center retrospective cohort study of patients with CVD and SUD on a GLP-1 agonist. As previous studies have shown that change in body mass index (BMI) correlates with adherence to GLP-1 agonists, we stratified subjects by change in BMI over a two-year study period. Using SPSS, we analyzed number of hospital visits and conducted frequency analyses by type of CVD, type of SUD, and change in BMI during our study period.
Results:
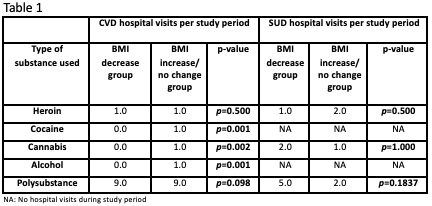
The study population consists of 81 patients on GLP-1 agonists who have SUD and CVD. BMI decreased in 55 patients (67.9%), increased in 24 patients (29.6%), and remained the same in 2 patients (2.5%). Correlation analysis was conducted between change in BMI and the number of hospital visits related to SUD and CVD, indicating positive correlation between change in BMI and reduction in hospital visits related to both SUD (r=0.136, p= 0.230) and CVD (r=0.142, p= 0.208). Subgroup analyses were also performed by specific SUD type; patients with cocaine, cannabinoid, or alcohol use disorders had decreased hospital visits related to CVD (p<0.05) while those with opioid or polysubstance use disorders did not (Table 1).
Conclusion:
GLP-1 agonists, previously established to reduce adverse CVD outcomes, may be especially beneficial in patients with both CVD and SUD. More research is needed to determine how to optimize the benefit from treatment with GLP-1 agonists in this vulnerable patient population.
Improved outcomes related to the use of glucagon-like peptide 1 (GLP-1) agonists in patients with cardiovascular disease (CVD) have been well documented. Small studies have shown benefits of GLP-1 agonists in reducing substance use in patients with substance use disorders (SUDs). In patients with CVD, co-occurring SUDs are known to worsen outcomes. The use of GLP-1 agonists to improve outcomes related to both CVD and SUD could improve healthcare disparities in this marginalized population.
Hypothesis:
The use of GLP-1 agonists in patients with CVD and SUD could improve outcomes related to both disease processes.
Aim:
Our aim is to describe clinical outcomes in patients with CVD and SUD who were prescribed GLP-1 agonists.
Methods:
This is a single-center retrospective cohort study of patients with CVD and SUD on a GLP-1 agonist. As previous studies have shown that change in body mass index (BMI) correlates with adherence to GLP-1 agonists, we stratified subjects by change in BMI over a two-year study period. Using SPSS, we analyzed number of hospital visits and conducted frequency analyses by type of CVD, type of SUD, and change in BMI during our study period.
Results:
The study population consists of 81 patients on GLP-1 agonists who have SUD and CVD. BMI decreased in 55 patients (67.9%), increased in 24 patients (29.6%), and remained the same in 2 patients (2.5%). Correlation analysis was conducted between change in BMI and the number of hospital visits related to SUD and CVD, indicating positive correlation between change in BMI and reduction in hospital visits related to both SUD (r=0.136, p= 0.230) and CVD (r=0.142, p= 0.208). Subgroup analyses were also performed by specific SUD type; patients with cocaine, cannabinoid, or alcohol use disorders had decreased hospital visits related to CVD (p<0.05) while those with opioid or polysubstance use disorders did not (Table 1).
Conclusion:
GLP-1 agonists, previously established to reduce adverse CVD outcomes, may be especially beneficial in patients with both CVD and SUD. More research is needed to determine how to optimize the benefit from treatment with GLP-1 agonists in this vulnerable patient population.
More abstracts on this topic:
Adverse Childhood Experiences (ACEs) and Cardiovascular Health: Future of Families and Child Wellbeing Study (FFCWS)
__PRESENT
__PRESENT
Pedamallu Havisha, Van Horn Linda, Stein James, Korcarz Claudia, Hansen Kristin, Mitchell Colter, Heard-garris Nia, Lloyd-jones Donald, Allen Norrina, Gauen Abigail, Ning Hongyan, Wilkins John, Goldman Noreen, Notterman Daniel, Hou Lifang, Zheng Yinan, Marma Amanda
10-Year Trends in Last Known Well to Arrival Time in Acute Ischemic Stroke Patients: 2014-2023Ferrone Nicholas, Sanmartin Maria, O'hara Joseph, Jimenez Jean, Ferrone Sophia, Wang Jason, Katz Jeffrey, Sanelli Pina