Final ID: Su4095
Mechanical Circulatory Support in Cardiogenic Shock Secondary to Acute Myocardial Infarction: A Systematic Review and Network Meta-analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background
Cardiogenic shock is a leading cause of mortality in acute myocardial infarction. The efficacy of mechanical circulatory support devices in reducing mortality is uncertain.
Research Question
Which mechanical circulatory support device is associated with lower mortality and better safety outcomes in patients with cardiogenic shock?
Goals/Aims
To compare different mechanical circulatory support devices in patients with cardiogenic shock.
Methods
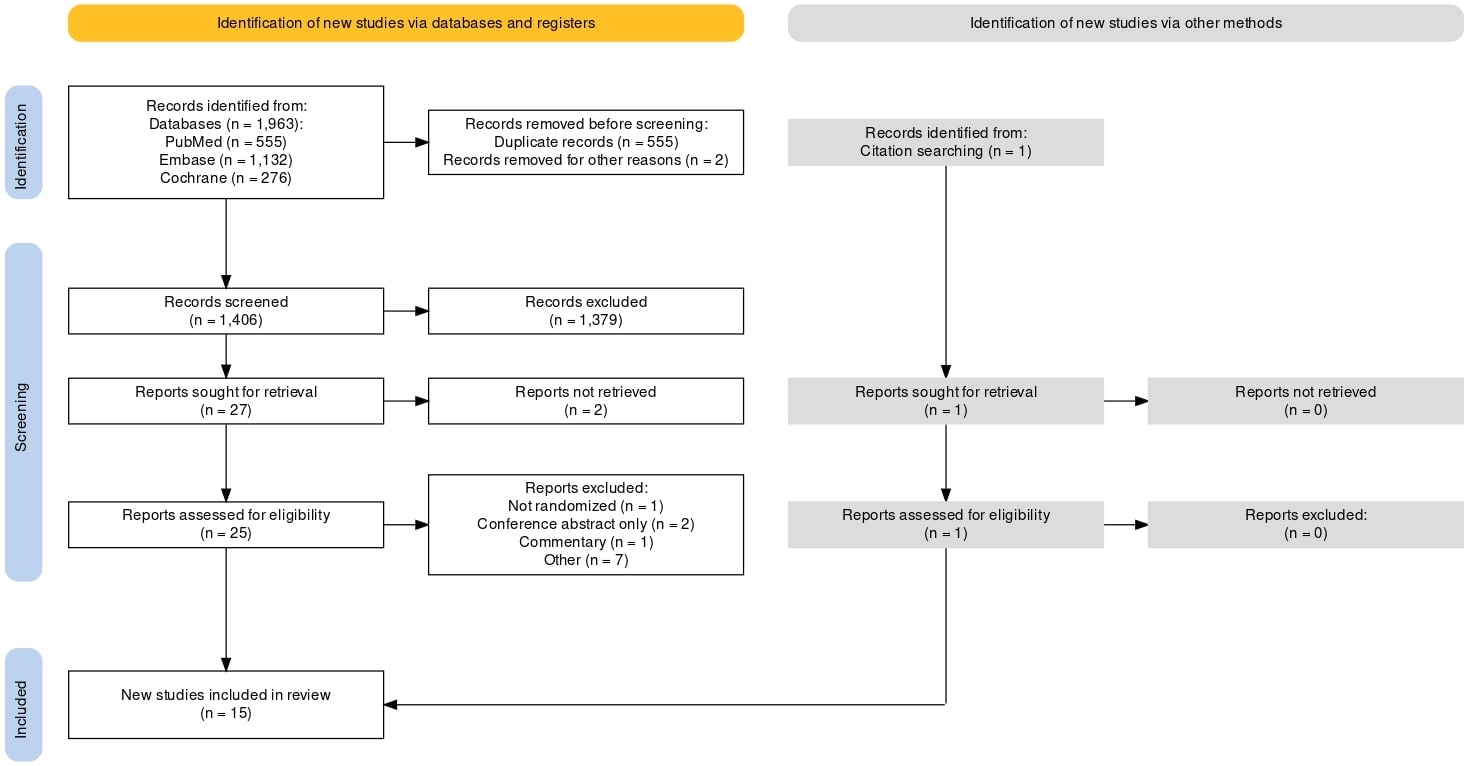
We conducted a systematic search of PubMed, Embase, and Cochrane Library databases up to April 2024 for randomized controlled trials (RCTs) involving mechanical circulatory support devices (e.g., Impella, ECMO, IABP, percutaneous ventricular assist device) reporting at least 30-day mortality or safety outcomes (bleeding, cerebrovascular events, sepsis). Two reviewers independently extracted data on mortality and safety outcomes. A frequentist network meta-analysis with random-effects models was used, calculating risk ratios (RR) with 95% confidence intervals (CI) and treatment ranking probabilities (P-SCORE).
Results
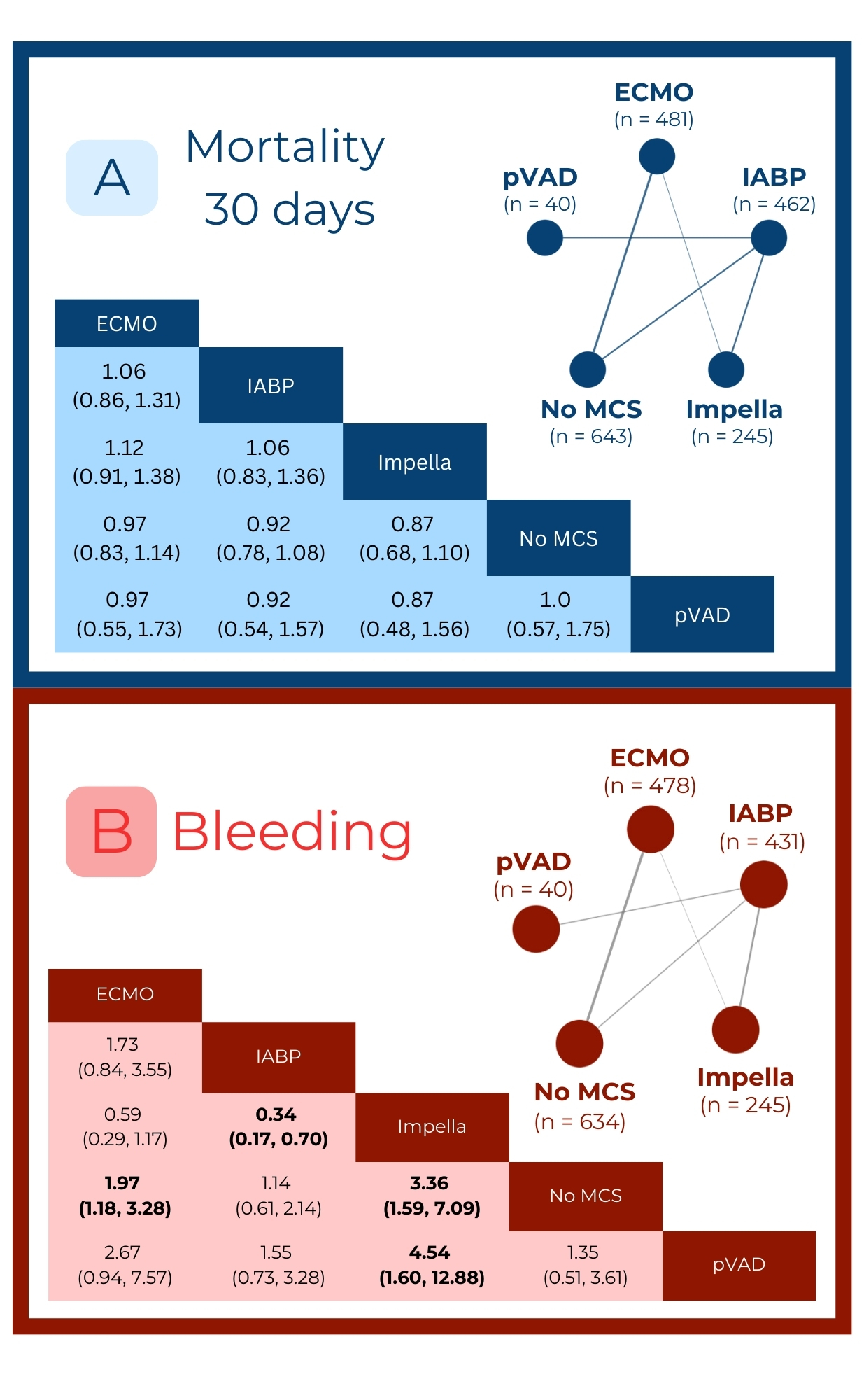
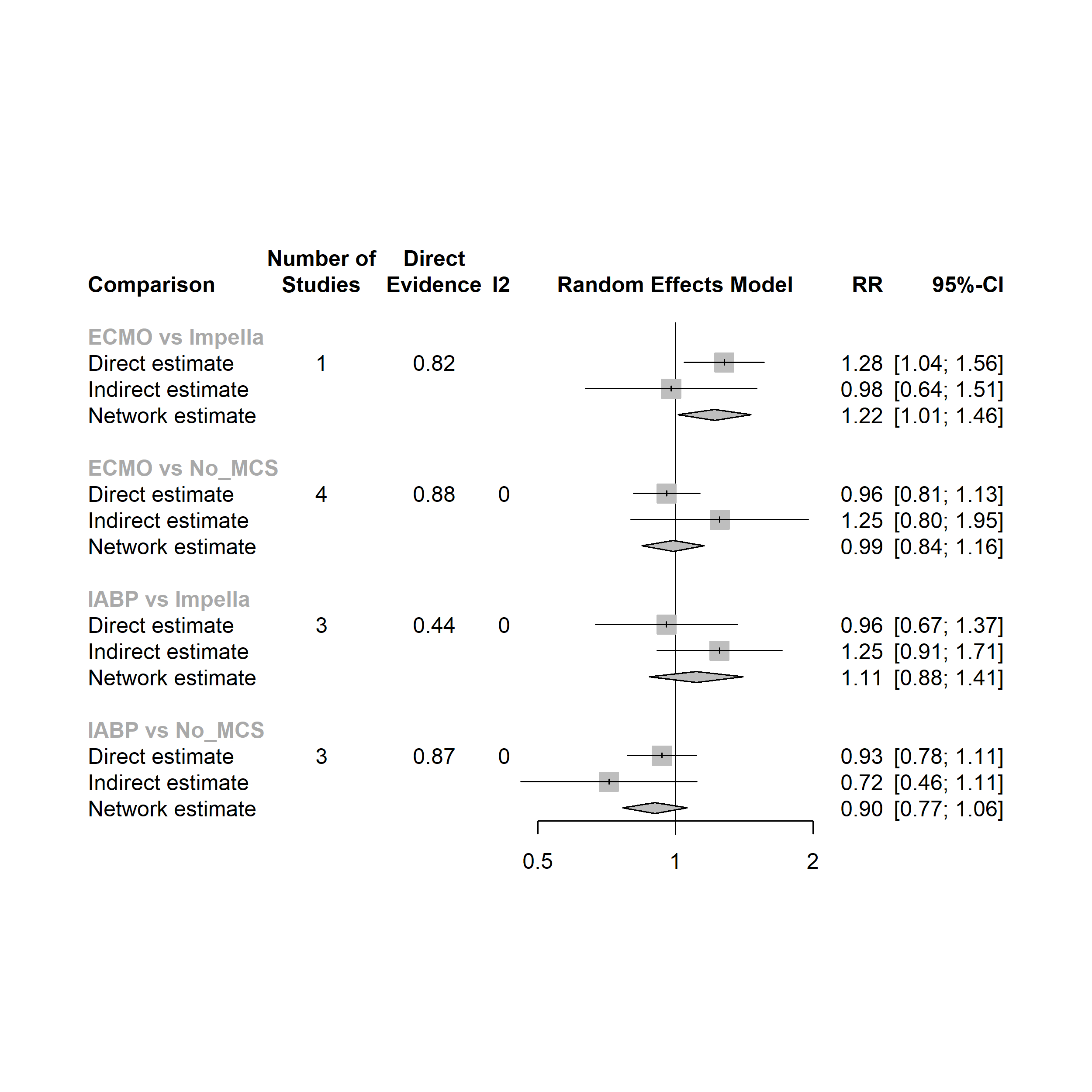
Our systematic review and network meta-analysis included 15 RCTs, involving 1,927 patients, comprised of 77.6% of males with a mean age of 63.1 years, from Europe, North America, and Asia. No device reduced 30-day mortality. IABP had a lower risk of bleeding compared with Impella (RR 0.34; 95% CI 0.17-0.7), while ECMO had a higher bleeding risk compared with no support (RR 1.97; 95% CI 1.18-3.28). Regarding long-term mortality (30 + 180 days), ECMO showed a higher risk compared with Impella (RR 1.22; 95% CI 1.01-1.46). IABP led to fewer cerebrovascular events (RR 0.37; 95% CI 0.15-0.93) and sepsis (RR 0.54; 95% CI 0.35-0.83) compared with Impella. No significant differences were found in other comparisons.
Conclusion
No mechanical circulatory support device significantly reduced 30-day mortality in patients with cardiogenic shock. IABP was associated with lower risks of bleeding, cerebrovascular events, and sepsis compared with Impella. ECMO showed a higher risk of bleeding compared with no support and higher long-term mortality compared with Impella. Further research should focus on identifying safer strategies and optimal patient profiles for these devices to improve outcomes.
Cardiogenic shock is a leading cause of mortality in acute myocardial infarction. The efficacy of mechanical circulatory support devices in reducing mortality is uncertain.
Research Question
Which mechanical circulatory support device is associated with lower mortality and better safety outcomes in patients with cardiogenic shock?
Goals/Aims
To compare different mechanical circulatory support devices in patients with cardiogenic shock.
Methods
We conducted a systematic search of PubMed, Embase, and Cochrane Library databases up to April 2024 for randomized controlled trials (RCTs) involving mechanical circulatory support devices (e.g., Impella, ECMO, IABP, percutaneous ventricular assist device) reporting at least 30-day mortality or safety outcomes (bleeding, cerebrovascular events, sepsis). Two reviewers independently extracted data on mortality and safety outcomes. A frequentist network meta-analysis with random-effects models was used, calculating risk ratios (RR) with 95% confidence intervals (CI) and treatment ranking probabilities (P-SCORE).
Results
Our systematic review and network meta-analysis included 15 RCTs, involving 1,927 patients, comprised of 77.6% of males with a mean age of 63.1 years, from Europe, North America, and Asia. No device reduced 30-day mortality. IABP had a lower risk of bleeding compared with Impella (RR 0.34; 95% CI 0.17-0.7), while ECMO had a higher bleeding risk compared with no support (RR 1.97; 95% CI 1.18-3.28). Regarding long-term mortality (30 + 180 days), ECMO showed a higher risk compared with Impella (RR 1.22; 95% CI 1.01-1.46). IABP led to fewer cerebrovascular events (RR 0.37; 95% CI 0.15-0.93) and sepsis (RR 0.54; 95% CI 0.35-0.83) compared with Impella. No significant differences were found in other comparisons.
Conclusion
No mechanical circulatory support device significantly reduced 30-day mortality in patients with cardiogenic shock. IABP was associated with lower risks of bleeding, cerebrovascular events, and sepsis compared with Impella. ECMO showed a higher risk of bleeding compared with no support and higher long-term mortality compared with Impella. Further research should focus on identifying safer strategies and optimal patient profiles for these devices to improve outcomes.
More abstracts on this topic:
A recombinant protein oxygen carrier with reduced nitric oxide scavenging as a blood substitute for resuscitation
Xu Qinzi, Rochon Elizabeth, Bocian Kaitlin, Huang Xue, Poropatich Ronald, Gladwin Mark, Tejero Jesus, Rose Jason, Rodriguez Deborah, Hwang Hyon, Turner Bryan, Hunt Thomas, Dent Matthew, Demartino Anthony, Abdelghany Youmna, Chen Xiukai
A Meta-Analysis Comparing Same-Day Discharge to Later-Day Discharge in Transcatheter Aortic Valve ReplacementJain Hritvik, Passey Siddhant, Jain Jyoti, Goyal Aman, Wasir Amanpreet, Ahmed Mushood, Patel Nandan, Yadav Ashish, Shah Janhvi, Mehta Aryan