Final ID: Mo4034
Predictors of Mortality Among Hospitalized Patients with Acute Myocardial Infarction by Systemic Lupus Erythematosus Diagnosis
Abstract Body (Do not enter title and authors here): Introduction:
Studies have reported on the prevalence, and associations between acute myocardial infarction (AMI) and systemic lupus erythematosus (SLE), but there is limited data on the predictors of mortality and whether these differ among patients with a diagnosis of SLE. We examined the factors associated with mortality among hospitalized patients with a diagnosis of AMI with or without SLE.
Hypothesis:
Patient and hospital associated factors can predict mortality among hospitalized patients with AMI and these predictors differ by SLE diagnosis
Methods:
The National Inpatient Sample (NIS) data collected from 2016 – 2020 was utilized to conduct retrospective cohort analyses. Multivariate logistic regression models were used to examine the factors associated with mortality among hospitalized patients with AMI by SLE diagnosis.
Results:
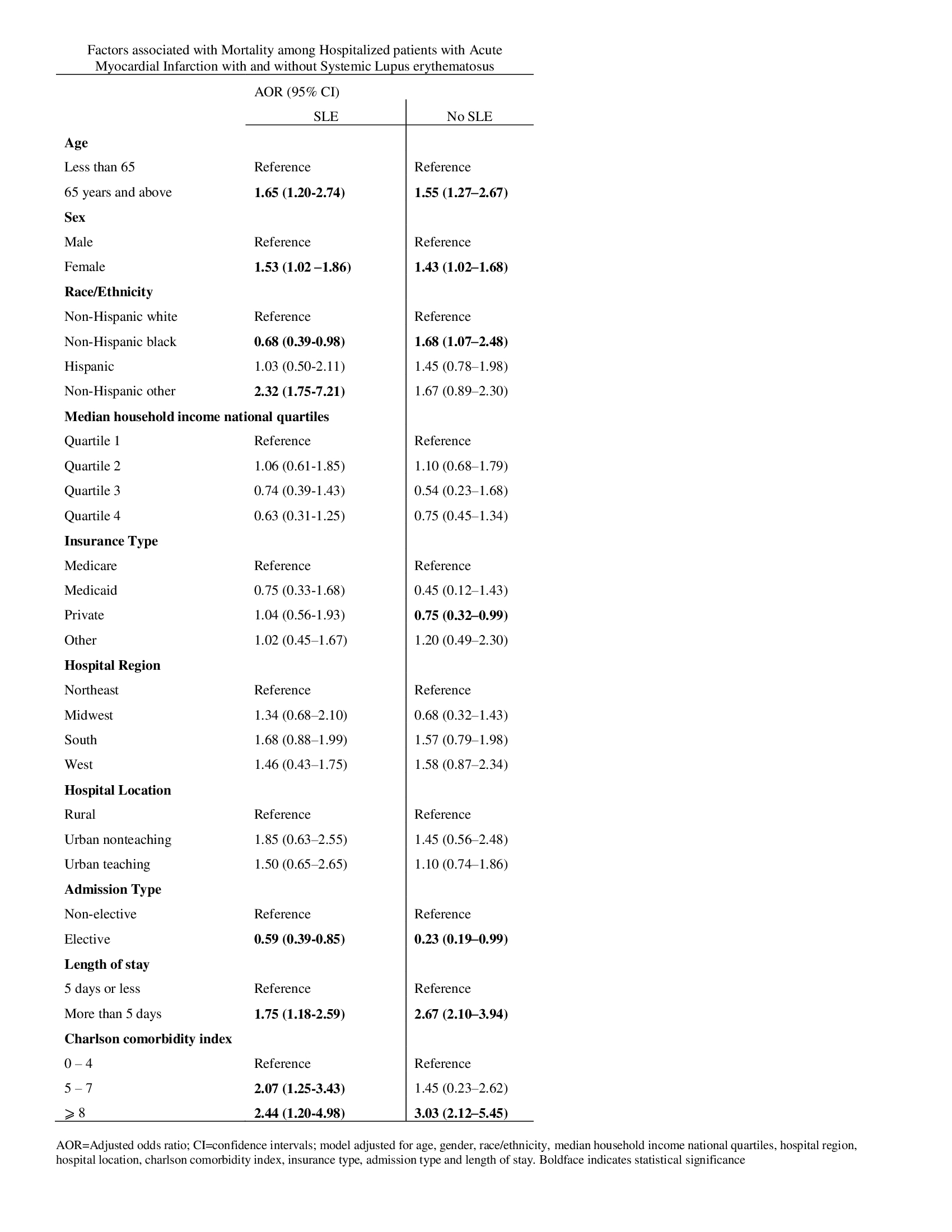
Among SLE patients with a diagnosis of AMI, being female (AOR: 1.53; 95% CI: 1.02-1.86) and 65 years and above (AOR: 1.65; 95% CI: 1.20-2.74) was associated with higher odds of mortality compared to being male and younger than 65 years. Elective admission (AOR: 0.59; 95% CI: 0.39-0.85) was associated with lower risk of mortality relative to non-elective admission. Of note, non-Hispanic blacks (AOR: 0.68; 95% CI: 0.39-0.98) had lower odds of mortality than non-Hispanic whites. Patients with length of stay greater than 5 days (AOR: 1.75; 95% CI: 1.18-2.59) were more likely to die than those with hospital stay 5 days or less. Higher comorbidity scores were also associated with higher odds of mortality. Among patients without SLE, non-Hispanic blacks (AOR: 1.68; 95% CI: 1.07–2.48) reported higher mortality compared to their non-Hispanic white counterparts. Additionally, being on private insurance (AOR: 0.75; 95% CI: 0.32–0.99) was associated with lower odds of mortality relative to Medicare insurance.
Conclusion:
Our study highlights patients and hospital related factors that can predict mortality among patients hospitalized with AMI by SLE. Further studies are needed to explore these factors as it will help physicians identify patients that need closer monitoring.
Studies have reported on the prevalence, and associations between acute myocardial infarction (AMI) and systemic lupus erythematosus (SLE), but there is limited data on the predictors of mortality and whether these differ among patients with a diagnosis of SLE. We examined the factors associated with mortality among hospitalized patients with a diagnosis of AMI with or without SLE.
Hypothesis:
Patient and hospital associated factors can predict mortality among hospitalized patients with AMI and these predictors differ by SLE diagnosis
Methods:
The National Inpatient Sample (NIS) data collected from 2016 – 2020 was utilized to conduct retrospective cohort analyses. Multivariate logistic regression models were used to examine the factors associated with mortality among hospitalized patients with AMI by SLE diagnosis.
Results:
Among SLE patients with a diagnosis of AMI, being female (AOR: 1.53; 95% CI: 1.02-1.86) and 65 years and above (AOR: 1.65; 95% CI: 1.20-2.74) was associated with higher odds of mortality compared to being male and younger than 65 years. Elective admission (AOR: 0.59; 95% CI: 0.39-0.85) was associated with lower risk of mortality relative to non-elective admission. Of note, non-Hispanic blacks (AOR: 0.68; 95% CI: 0.39-0.98) had lower odds of mortality than non-Hispanic whites. Patients with length of stay greater than 5 days (AOR: 1.75; 95% CI: 1.18-2.59) were more likely to die than those with hospital stay 5 days or less. Higher comorbidity scores were also associated with higher odds of mortality. Among patients without SLE, non-Hispanic blacks (AOR: 1.68; 95% CI: 1.07–2.48) reported higher mortality compared to their non-Hispanic white counterparts. Additionally, being on private insurance (AOR: 0.75; 95% CI: 0.32–0.99) was associated with lower odds of mortality relative to Medicare insurance.
Conclusion:
Our study highlights patients and hospital related factors that can predict mortality among patients hospitalized with AMI by SLE. Further studies are needed to explore these factors as it will help physicians identify patients that need closer monitoring.
More abstracts on this topic:
A Contemporary Machine Learning-Based Risk Stratification for Mortality and Hospitalization in Heart Failure with Preserved Ejection Fraction Using Multimodal Real-World Data
Fudim Marat, Weerts Jerremy, Patel Manesh, Balu Suresh, Hintze Bradley, Torres Francisco, Micsinai Balan Mariann, Rigolli Marzia, Kessler Paul, Touzot Maxime, Lund Lars, Van Empel Vanessa, Pradhan Aruna, Butler Javed, Zehnder Tobias, Sauty Benoit, Esposito Christian, Balazard Félix, Mayer Imke, Hallal Mohammad, Loiseau Nicolas
A Rare Cause of a Classic Presentation of NSTEMI: Case of 39-Year-Old Female with Hypothyroidism Induced MyocarditisQuadri Fayz, Qazi Mariam, Teague Taylor