Final ID: Su2132
Trends in 30-Day Readmission Rate, Mortality Outcome and Resources Utilization Among Patient who underwent Leadless Pacemaker Revision and Removal.
Abstract Body (Do not enter title and authors here): Background: Leadless pacemakers (LPM) utilization has grown significantly, yet data on LPM removal and/or revision (LPM-RR) remains limited. This study aims to evaluate trends in 30-day readmission rate (30-dRr), mortality, and resource utilization associated with LPM-RR
Method: We analyzed data from the Nationwide Readmission Database from 2016 to 2021. Patients ≥ 18 years who underwent LPM-RR were identified using ICD-10 codes. The primary outcome was the trend on 30-dRr following LPM-RR. Secondary outcomes included mortality, resource utilization (Length of stay {LOS} & inflation-adjusted mean hospital cost), & most common readmission diagnosis. Predictive marginal effects over the years & regression analyses were conducted.
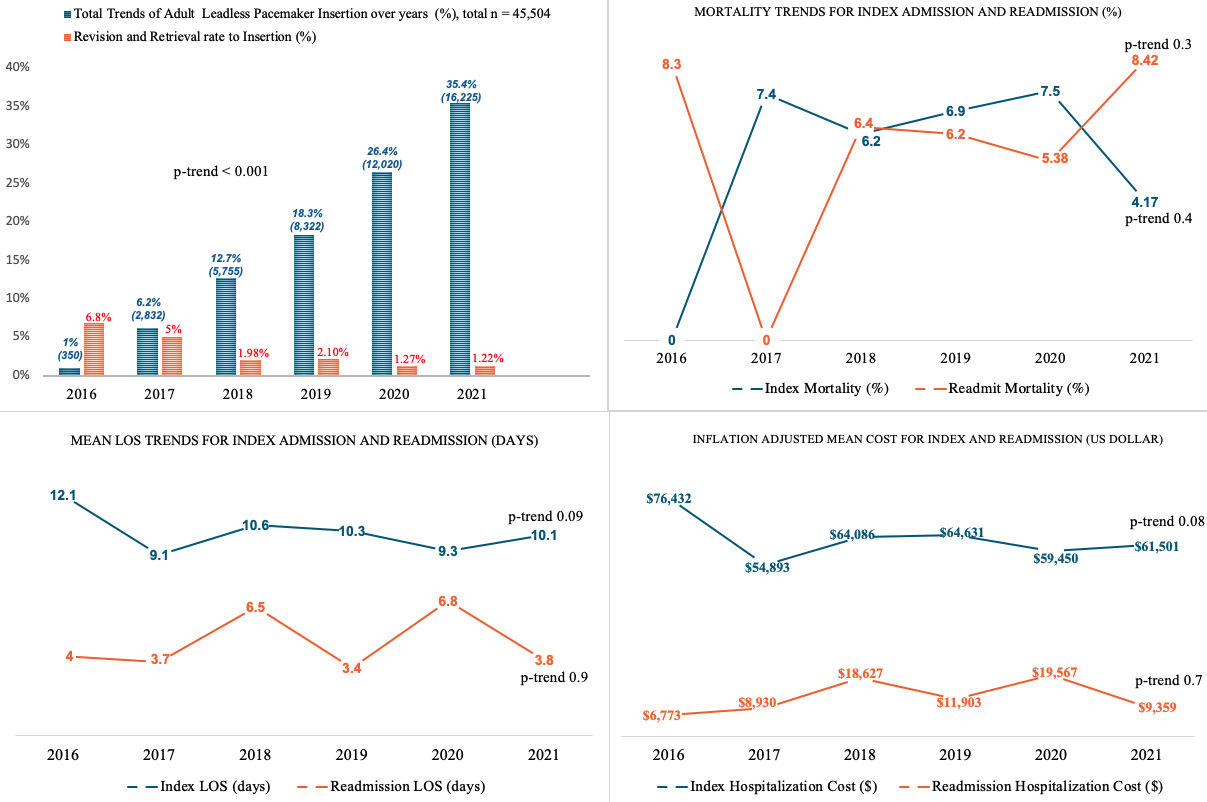
Results: LPMs placement increased from 350 in 2016 to 16,225 in 2021 (p-trend < 0.001), while the rate of revisions and removals declined from 6.2% to 1.2% (p-trend < 0.001). The mean age at index admission was 70.9 years with 51.6% females, compared to 71.6 years and 60.8% males among readmitted patients. The 30-dRr increased slightly from 13.8% in 2016 to 16% in 2021 (p trend = 0.1). Index admission mortality trends were non-significant, decreasing from 7.4% in 2017 to 4.2% in 2021 (p-trend = 0.4). Readmission mortality trends also remained non-significant, from 8.3% in 2016 to 8.4% in 2021 (p-trend = 0.3). The index admission mean LOS was 12.1 days in 2016 to 10.2 days in 2021 (p trend = 0.09), while readmission mean LOS was 4.1 days to 3.8 days (p trend = 0.9). The inflation-adjusted mean hospital cost for index admissions decreased from $76,432.5 in 2016 to $61,501 in 2021 (p trend = 0.08), whereas readmission costs increased from $6,773 to $9,358 (p-trend = 0.7). The most common reason for readmission was hypertensive heart disease with heart failure.
Conclusion: From 2016 to 2021, LPM implantation grew rapidly with a significant decline in revision and removal rates. During this period, 30-dRr & resource utilization have remained relatively stable, with a trend toward decreasing mortality within 30 days after LPM implantation, likely owing to technology/technique advancements, increased experience, as well as patient selection. Further research is needed to assess outcomes for the rapidly evolving use of LPM in an increasingly broader range of patient populations.
Method: We analyzed data from the Nationwide Readmission Database from 2016 to 2021. Patients ≥ 18 years who underwent LPM-RR were identified using ICD-10 codes. The primary outcome was the trend on 30-dRr following LPM-RR. Secondary outcomes included mortality, resource utilization (Length of stay {LOS} & inflation-adjusted mean hospital cost), & most common readmission diagnosis. Predictive marginal effects over the years & regression analyses were conducted.
Results: LPMs placement increased from 350 in 2016 to 16,225 in 2021 (p-trend < 0.001), while the rate of revisions and removals declined from 6.2% to 1.2% (p-trend < 0.001). The mean age at index admission was 70.9 years with 51.6% females, compared to 71.6 years and 60.8% males among readmitted patients. The 30-dRr increased slightly from 13.8% in 2016 to 16% in 2021 (p trend = 0.1). Index admission mortality trends were non-significant, decreasing from 7.4% in 2017 to 4.2% in 2021 (p-trend = 0.4). Readmission mortality trends also remained non-significant, from 8.3% in 2016 to 8.4% in 2021 (p-trend = 0.3). The index admission mean LOS was 12.1 days in 2016 to 10.2 days in 2021 (p trend = 0.09), while readmission mean LOS was 4.1 days to 3.8 days (p trend = 0.9). The inflation-adjusted mean hospital cost for index admissions decreased from $76,432.5 in 2016 to $61,501 in 2021 (p trend = 0.08), whereas readmission costs increased from $6,773 to $9,358 (p-trend = 0.7). The most common reason for readmission was hypertensive heart disease with heart failure.
Conclusion: From 2016 to 2021, LPM implantation grew rapidly with a significant decline in revision and removal rates. During this period, 30-dRr & resource utilization have remained relatively stable, with a trend toward decreasing mortality within 30 days after LPM implantation, likely owing to technology/technique advancements, increased experience, as well as patient selection. Further research is needed to assess outcomes for the rapidly evolving use of LPM in an increasingly broader range of patient populations.
More abstracts on this topic:
A Model-Sharing Approach for Quality Improvement of Diabetes and Cardiovascular Disease
Elligers Kyle, Pollner Meghan, Overton Katherine, Congdon Michelle, Greenway Stacey, Lambro Patricia, Sadiku Steven, Schechter Rona, Whelan John, Pressley Bianca, Sednew Renee, Duckett Sara
A Hospital-Wide Multidimensional Approach to Pediatric In-Hospital Cardiac Arrest Review: Early Identification and PreventionLoeb Daniel, Collins Kelly, Ortega Karina, Dewan Maya