Final ID: MDP546
Postprocedural Anticoagulation Following Primary Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction: A Meta-Analysis of Clinical Outcomes
Abstract Body (Do not enter title and authors here): Background: The use of procedural anticoagulation during primary percutaneous coronary intervention (PCI) is well established and has been shown to improve clinical outcomes in patients with ST-elevation myocardial infarction (STEMI). Despite its widespread application in clinical settings, the necessity and efficacy of postprocedural anticoagulation (PPA) remain contentious. Thus, this is the first meta-analysis to assess the efficacy and safety of PPA after PCI for the management of STEMI.
Methods: A comprehensive search of PubMed, Cochrane, and Embase databases was conducted to identify studies comparing the clinical outcomes between PPA administration and control (placebo or no anticoagulant infusion) following PCI for STEMI treatment. Statistical analyses were performed using RevMan version 5.4.1, employing a random-effects model to calculate odds ratios (ORs) and their 95% confidence intervals (CIs).
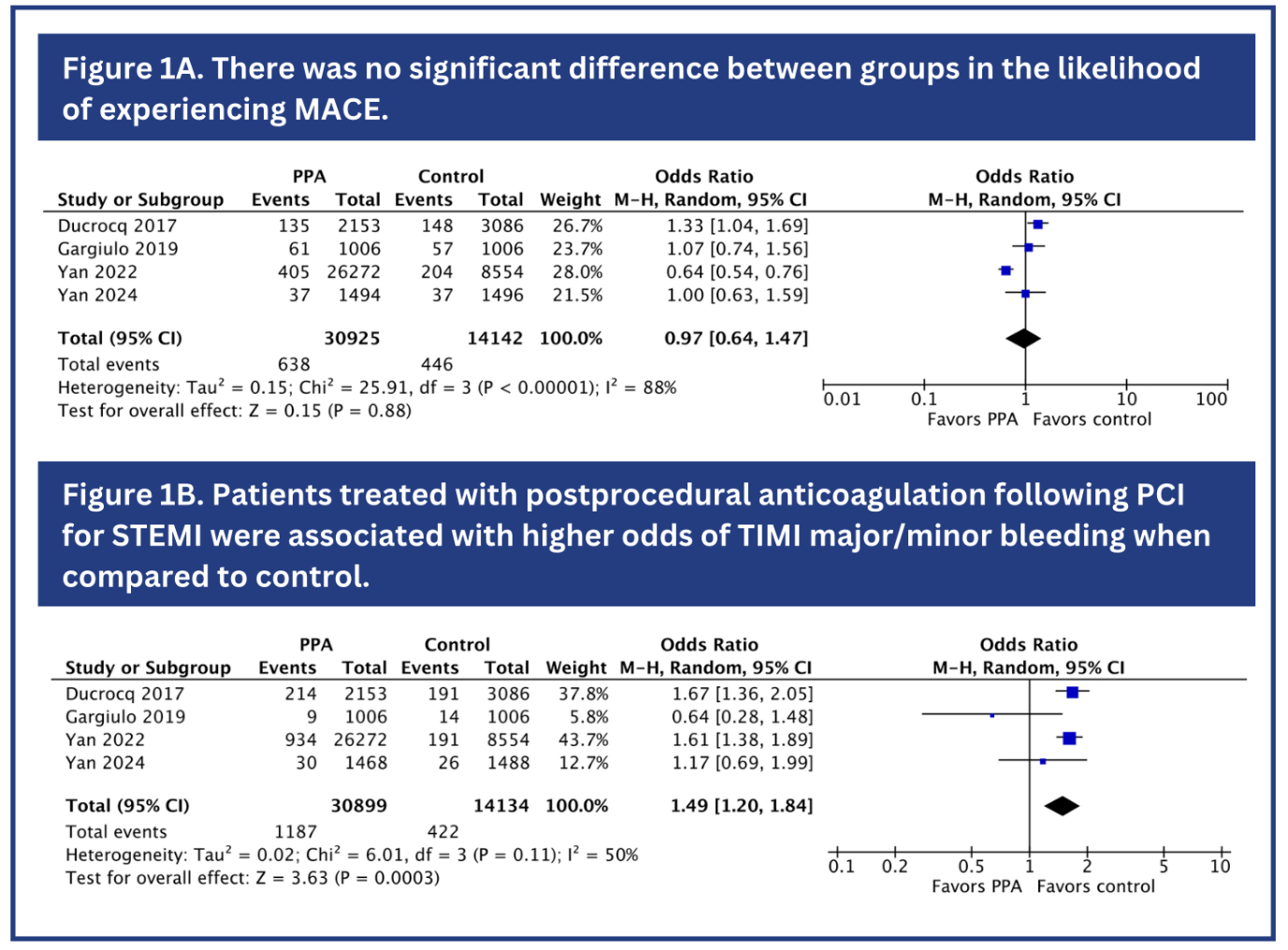
Results: A total of four studies comprising 45,066 patients were included (2 RCTs and 2 non-randomized studies), of which 30,925 (68.6%) received PPA. Among the included patients, 35,770 (79.4%) were female. Compared to the control group, PPA did not significantly reduce all-cause mortality (OR 0.82; 95% CI 0.49 – 1.36; P=0.44), cardiac death (OR 0.81; 95% CI 0.49 – 1.33; P=0.41), and major adverse cardiovascular events (MACE) (OR 0.97; 95% CI 0.64 – 1.47; P=0.88; Figure 1A). Moreover, the odds of stent thrombosis (OR 1.24; 95% CI 0.92 – 1.68; P=0.15), myocardial infarction (OR 1.03; 95% CI 0.79 – 1.36; P= 0.81) and stroke (OR 0.95; 95% CI 0.41 – 2.20; P=0.90) did not differ between the groups. However, patients receiving PPA were associated with higher odds of TIMI major/minor bleeding (OR 1.49; 95% CI 1.20 – 1.84; P<0.01; Figure 1B).
Conclusions: This meta-analysis reveals no significant differences in the odds of all-cause mortality, cardiac death, MACE, stent thrombosis, myocardial infarction and stroke between PPA and control following PCI for the management of STEMI. However, PPA was associated with higher odds of TIMI major/minor bleeding when compared to control. Further randomized controlled trials are warranted to corroborate these findings.
Methods: A comprehensive search of PubMed, Cochrane, and Embase databases was conducted to identify studies comparing the clinical outcomes between PPA administration and control (placebo or no anticoagulant infusion) following PCI for STEMI treatment. Statistical analyses were performed using RevMan version 5.4.1, employing a random-effects model to calculate odds ratios (ORs) and their 95% confidence intervals (CIs).
Results: A total of four studies comprising 45,066 patients were included (2 RCTs and 2 non-randomized studies), of which 30,925 (68.6%) received PPA. Among the included patients, 35,770 (79.4%) were female. Compared to the control group, PPA did not significantly reduce all-cause mortality (OR 0.82; 95% CI 0.49 – 1.36; P=0.44), cardiac death (OR 0.81; 95% CI 0.49 – 1.33; P=0.41), and major adverse cardiovascular events (MACE) (OR 0.97; 95% CI 0.64 – 1.47; P=0.88; Figure 1A). Moreover, the odds of stent thrombosis (OR 1.24; 95% CI 0.92 – 1.68; P=0.15), myocardial infarction (OR 1.03; 95% CI 0.79 – 1.36; P= 0.81) and stroke (OR 0.95; 95% CI 0.41 – 2.20; P=0.90) did not differ between the groups. However, patients receiving PPA were associated with higher odds of TIMI major/minor bleeding (OR 1.49; 95% CI 1.20 – 1.84; P<0.01; Figure 1B).
Conclusions: This meta-analysis reveals no significant differences in the odds of all-cause mortality, cardiac death, MACE, stent thrombosis, myocardial infarction and stroke between PPA and control following PCI for the management of STEMI. However, PPA was associated with higher odds of TIMI major/minor bleeding when compared to control. Further randomized controlled trials are warranted to corroborate these findings.
More abstracts on this topic:
A quality improvement intervention and academic detailing vs. academic detailing alone, a randomized quality improvement study
Sussman Jeremy, Evans Richard, Garlick Brittani, Barnes Geoffrey, Allen Arthur, Parra David, Burns Jennifer, Kurlander Jacob
Abbreviated Ticagrelor-Based Dual Antiplatelet Therapy in Acute Coronary Syndrome: A Systematic Review and Meta-AnalysisHarmouch Wissam, Elbadawi Ayman, Thakker Ravi, Khalid Umair, Khalife Wissam, Kleiman Neal, Rangasetty Umamahesh, Kayani Waleed, Jneid Hani, Al Hemyari Bashar