Final ID: Mo2096
Risk for appropriate ICD intervention and complications in patients implanted after an out-hospital cardiac arrest compared to patients implanted for primary and other secondary prevention indication
Abstract Body (Do not enter title and authors here): Background: it is unclear if patients implanted with an implantable cardioverter defibrillator (ICD) after an out-of-hospital cardiac arrest (OHCA) have a higher risk of appropriate device therapy than patients implanted for primary and other secondary prevention.
Aims: to assess if appropriate device interventions (ATP/shocks) are higher in patients implanted after OHCA compared to patients implanted for primary and secondary prevention other than OHCA. To verify also if mortality, implantation-related complications (pneumothorax, hemothorax, hematoma, cardiac tamponade), device-related complications (lead displacement and fracture, infections) and inappropriate shocks/ATP are higher in OHCA patients.
Methods: a retrospective multicenter international study. We included all the patients implanted with an ICD in 2015 and 2016 in the centers. Follow-up was concluded if death or at the last follow-up available until 12/2023. Patients were divided according to ICD indication (secondary prevention after OHCA, other secondary prevention, primary prevention).
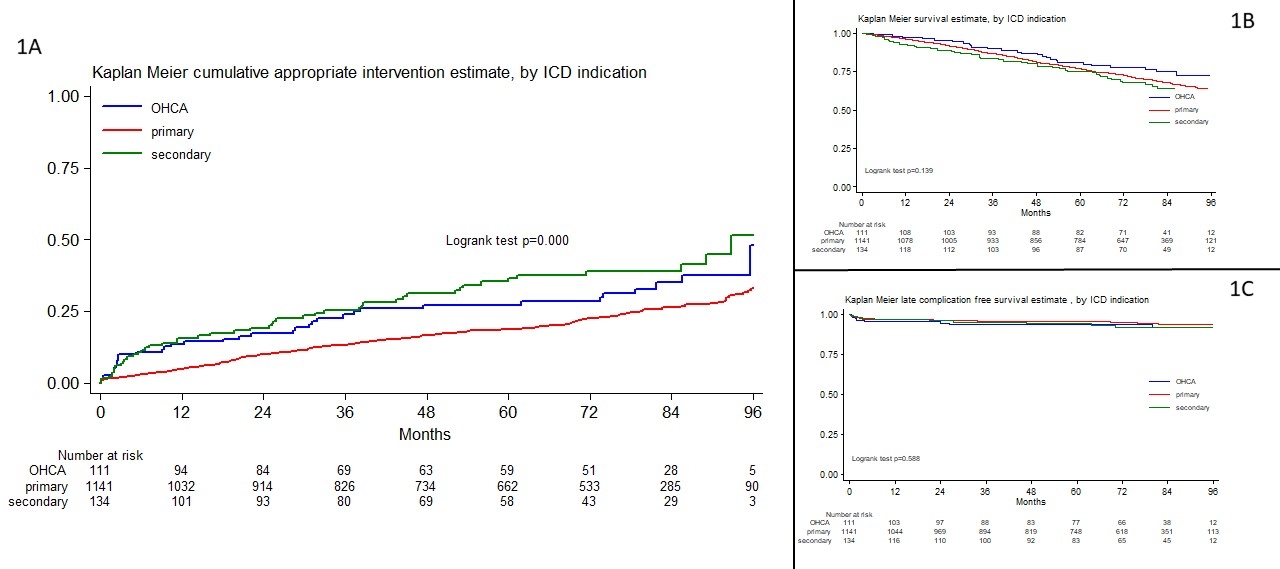
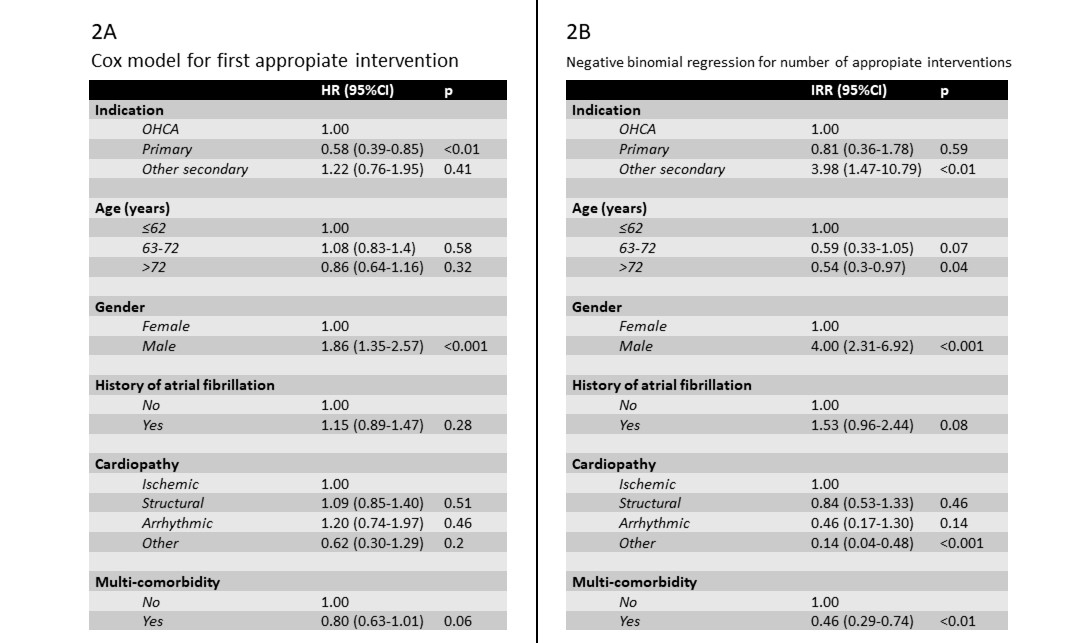
Results: 1386 patients (79% males; median age 67, IQR 59-74) from 15 centers were included (median follow-up 83 months): 111 patients in OHCA group, 134 in other secondary prevention group and 1141 in primary prevention group. Considering the first appropriate intervention, a significant difference among the three groups was observed (Fig.1A) and, at post-hoc comparison, the OHCA group was at higher risk than primary prevention (HR 1.51, 95%CI 1.06-2.17, p=0.02), but was at similar risk than other secondary prevention (HR 0.79, 95%CI 0.51-1.23, p=0.3). This was confirmed also after correction for age, gender, history of atrial fibrillation, aetiology and multi-comorbidity (Fig.2A). Considering the number of appropriate interventions during follow-up, the risk of OHCA group was lower than other secondary prevention (IRR 0.28, 95%CI 0.11-0.68, p<0.01) and similar to primary prevention (IRR 0.97, 95%CI 0.47-1.96, p=0.93), also after correction for the other predictors (Fig.2B). The three groups showed no differences in survival (Fig.1B), implantation-related complication, device-related complications (Fig.1C) and inappropriate shocks/ATP.
Conclusion: Our study highlights how OHCA patients represents a peculiar population with the same chance of survival and rate of complications compared to primary and other secondary prevention patients suggesting the need of more studies to improve their long-term treatment.
Aims: to assess if appropriate device interventions (ATP/shocks) are higher in patients implanted after OHCA compared to patients implanted for primary and secondary prevention other than OHCA. To verify also if mortality, implantation-related complications (pneumothorax, hemothorax, hematoma, cardiac tamponade), device-related complications (lead displacement and fracture, infections) and inappropriate shocks/ATP are higher in OHCA patients.
Methods: a retrospective multicenter international study. We included all the patients implanted with an ICD in 2015 and 2016 in the centers. Follow-up was concluded if death or at the last follow-up available until 12/2023. Patients were divided according to ICD indication (secondary prevention after OHCA, other secondary prevention, primary prevention).
Results: 1386 patients (79% males; median age 67, IQR 59-74) from 15 centers were included (median follow-up 83 months): 111 patients in OHCA group, 134 in other secondary prevention group and 1141 in primary prevention group. Considering the first appropriate intervention, a significant difference among the three groups was observed (Fig.1A) and, at post-hoc comparison, the OHCA group was at higher risk than primary prevention (HR 1.51, 95%CI 1.06-2.17, p=0.02), but was at similar risk than other secondary prevention (HR 0.79, 95%CI 0.51-1.23, p=0.3). This was confirmed also after correction for age, gender, history of atrial fibrillation, aetiology and multi-comorbidity (Fig.2A). Considering the number of appropriate interventions during follow-up, the risk of OHCA group was lower than other secondary prevention (IRR 0.28, 95%CI 0.11-0.68, p<0.01) and similar to primary prevention (IRR 0.97, 95%CI 0.47-1.96, p=0.93), also after correction for the other predictors (Fig.2B). The three groups showed no differences in survival (Fig.1B), implantation-related complication, device-related complications (Fig.1C) and inappropriate shocks/ATP.
Conclusion: Our study highlights how OHCA patients represents a peculiar population with the same chance of survival and rate of complications compared to primary and other secondary prevention patients suggesting the need of more studies to improve their long-term treatment.
More abstracts on this topic:
Clinical impact of new severe tricuspid regurgitation following device lead extraction
Arunachalam Karikalan Suganya, M Ezzedine Fatima, Desimone Christopher, Sugrue Alan, Padang Ratnasari, El Masry Hicham, Lee Justin, Deshmukh Abhishek, O'shea Michael, Vemulapalli Hema Srikanth, Mulpuru Siva, Killu Ammar, Siontis Konstantinos, Kowlgi Gurukripa, Cha Yong, Madhavan Malini
A-band titin-truncating variant promotes the development of arrhythmia-induced cardiomyopathy in a novel genetically-engineered porcine modelLee Kwonjae, Del Rio Carlos, Mcnally Elizabeth, Pfenniger Anna, Bhatnagar Ashita, Glinton Kristofor, Burrell Amy, Ober Rebecca, Mcluckie Alicia, Bishop Brian, Rogers Christopher, Geist Gail