Final ID: Su1135
Impact of Postprocedural Delirium on Inpatient Outcomes in Transcatheter Aortic Valve Replacement Patients: A Retrospective Propensity Matched Analysis
Abstract Body (Do not enter title and authors here):
Introduction
Transcatheter Aortic Valve Replacement (TAVR) is an increasingly common procedure for patients with severe aortic stenosis. However, postprocedural delirium remains a significant complication, impacting patient outcomes. This study aims to evaluate the inpatient outcomes of delirium in patients undergoing TAVR.
Methods
We performed a retrospective cohort study using the National Inpatient Sample 2018-2020, including patients who underwent TAVR with and without delirium. Propensity score matching was performed using the variables age, elective admission, sex, and comorbid conditions (congestive heart failure, cardiac arrhythmias, peripheral vascular disorders, hypertension, diabetes, chronic kidney disease, coagulopathy, and obesity) to compare patients with and without delirium. Weighted samples were utilized and p value <0.05 was considered significant.
Results
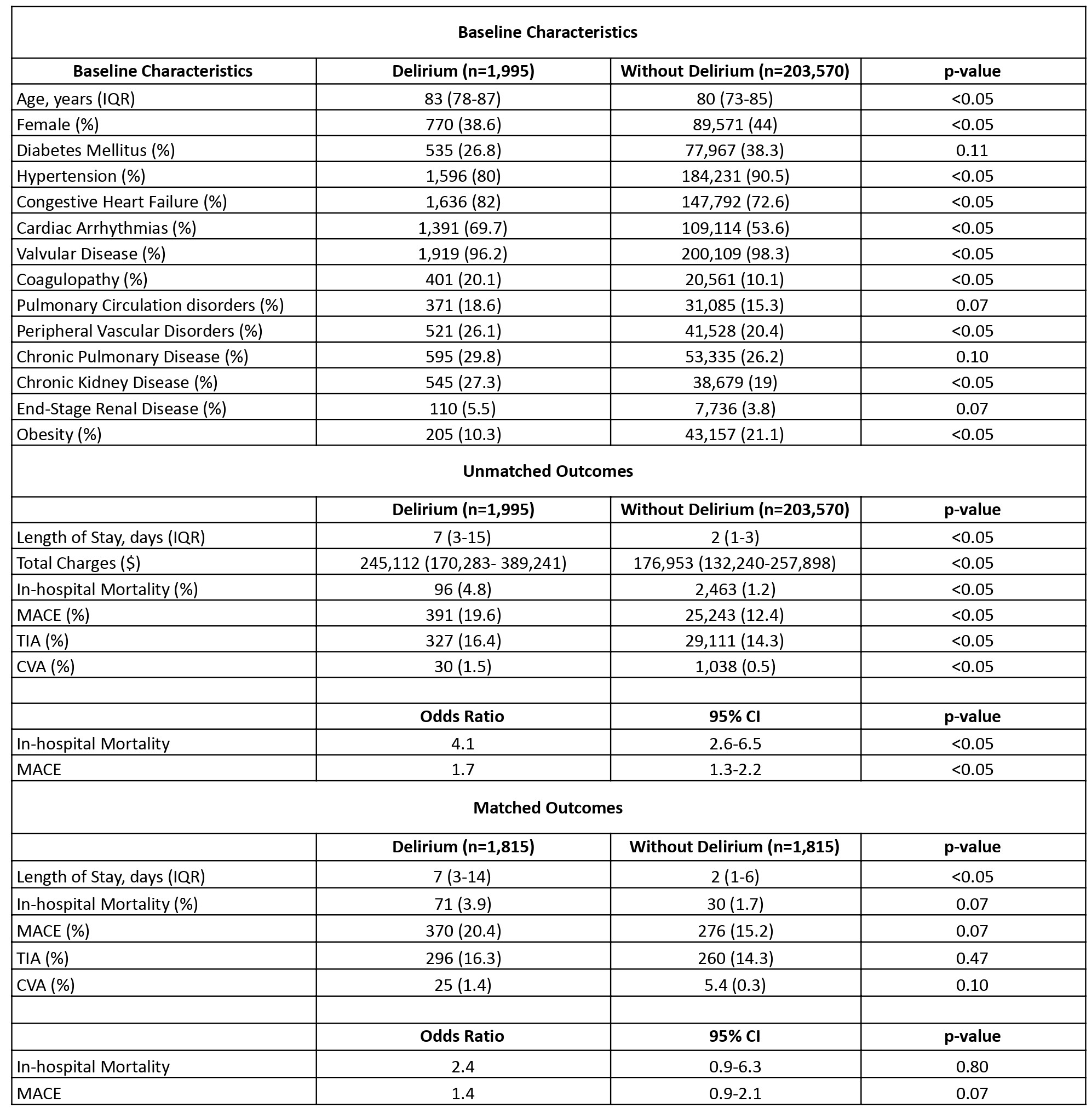
Out of 205,565 TAVR patients, 1,995 (0.97%) experienced delirium. Delirium was associated with older age (median age 83 vs. 80 years, p<0.05), higher prevalence of congestive heart failure, cardiac arrhythmias, valvular disease, and coagulopathy. Patients with delirium had significantly longer median LOS (7 (3-15) vs. 2 (1-3) days, p<0.05). Delirium was a significant predictor of in-hospital mortality (OR 4.08, 95% CI 2.55-6.52, p<0.05) and MACE (OR 1.72, 95% CI 1.34-2.21, p<0.05). After propensity score matching, delirium remained associated with increased median LOS (7 (3-14) vs. 2 (1-6) days, p<0.05); however, the difference in mortality (3.9% vs. 1.7%, p=0.07), and MACE (20.4% vs. 15.2%, p=0.06) became statistically insignificant after propensity matching. Detailed results are mentioned in Table 1.
Discussion
Our study highlights that delirium in TAVR patients is associated with significant adverse outcomes, including prolonged hospitalization, higher mortality and MACE rates compared to patients without delirium. The findings underscore the importance of identifying high-risk patients preoperatively and implementing strategies to mitigate delirium, thereby improving patient outcomes. Future research should focus on developing targeted interventions to prevent delirium in this vulnerable population.
Introduction
Transcatheter Aortic Valve Replacement (TAVR) is an increasingly common procedure for patients with severe aortic stenosis. However, postprocedural delirium remains a significant complication, impacting patient outcomes. This study aims to evaluate the inpatient outcomes of delirium in patients undergoing TAVR.
Methods
We performed a retrospective cohort study using the National Inpatient Sample 2018-2020, including patients who underwent TAVR with and without delirium. Propensity score matching was performed using the variables age, elective admission, sex, and comorbid conditions (congestive heart failure, cardiac arrhythmias, peripheral vascular disorders, hypertension, diabetes, chronic kidney disease, coagulopathy, and obesity) to compare patients with and without delirium. Weighted samples were utilized and p value <0.05 was considered significant.
Results
Out of 205,565 TAVR patients, 1,995 (0.97%) experienced delirium. Delirium was associated with older age (median age 83 vs. 80 years, p<0.05), higher prevalence of congestive heart failure, cardiac arrhythmias, valvular disease, and coagulopathy. Patients with delirium had significantly longer median LOS (7 (3-15) vs. 2 (1-3) days, p<0.05). Delirium was a significant predictor of in-hospital mortality (OR 4.08, 95% CI 2.55-6.52, p<0.05) and MACE (OR 1.72, 95% CI 1.34-2.21, p<0.05). After propensity score matching, delirium remained associated with increased median LOS (7 (3-14) vs. 2 (1-6) days, p<0.05); however, the difference in mortality (3.9% vs. 1.7%, p=0.07), and MACE (20.4% vs. 15.2%, p=0.06) became statistically insignificant after propensity matching. Detailed results are mentioned in Table 1.
Discussion
Our study highlights that delirium in TAVR patients is associated with significant adverse outcomes, including prolonged hospitalization, higher mortality and MACE rates compared to patients without delirium. The findings underscore the importance of identifying high-risk patients preoperatively and implementing strategies to mitigate delirium, thereby improving patient outcomes. Future research should focus on developing targeted interventions to prevent delirium in this vulnerable population.
More abstracts on this topic:
Clinical Outcomes of Postoperative Atrial Fibrillation Following Non-Cardiovascular Procedures: A Three-Year Study
Thangjui Sittinun, Abdelazeem Basel, Al Hajji Mohamed, Perkowski Gregory, Watson Hangyu, Santer Matthew, Thyagaturu Harshith, Balla Sudarshan, Arora Sandeep
Age-Related Differences in Aortic Valve Calcium Progression and the Risk for Aortic Stenosis: Multi-Ethnic Study of AtherosclerosisMarrero Natalie, Thanassoulis George, Rotter Jerome, Blaha Michael, Whelton Seamus, Jha Kunal, Grant Jelani, Razavi Alexander, Budoff Matthew, Shah Sanjiv, Blumenthal Roger, Post Wendy, Shaw Leslee