Final ID: Su2161
Effects of Empagliflozin on cardio-renal interaction in heart failure: Results from the CINNAMON-study and in-vivo experiments
Abstract Body (Do not enter title and authors here): Background and Purpose: Heart failure is associated with renal dysfunction suggesting a pathophysiological link between heart and kidney. Empagliflozin, a SGLT2 inhibitor, showed beneficial effects on both cardiovascular and renal endpoints. However, mechanistically, it is unclear if empagliflozin-dependent kidney protection is mediated via inhibition of tubular SGLT2 or more indirectly via improved cardiac function.
We hypothesized that Empagliflozin treatment improves left ventricular ejection fraction (LVEF) and thereby renal function in patients and mice independent of renal SGLT2 inhibition.
Methods: We evaluated LVEF and GFR in our patients with HF with reduced (n=32) and preserved ejection fraction (n=59) after 30 and 180 days (prospective, single-arm CINNAMON-study, DRKS00031101). Furthermore, we conducted transverse aortic constriction (TAC) in C57BL/6J (wildtype, WT) and SGLT2 deficient mice (SGLT2-KO). Animals received either Empagliflozin (10 mg/kg bw) or vehicle. Cardiac function was evaluated by echocardiography and kidney function by FITC-Sinistrin measurement (GFR).
Results: Empagliflozin treatment improved LVEF in patients with reduced LVEF whereas in patients with preserved LVEF (Fig. A, B) there was no change in LVEF (Fig. C). Interestingly, only in patients with LVEF < 40% there was a parallel improvement in GFR (Fig. D, E), whereas in patients with LVEF > 40% we only observed the well-known transient drop of GFR (Fig. F).
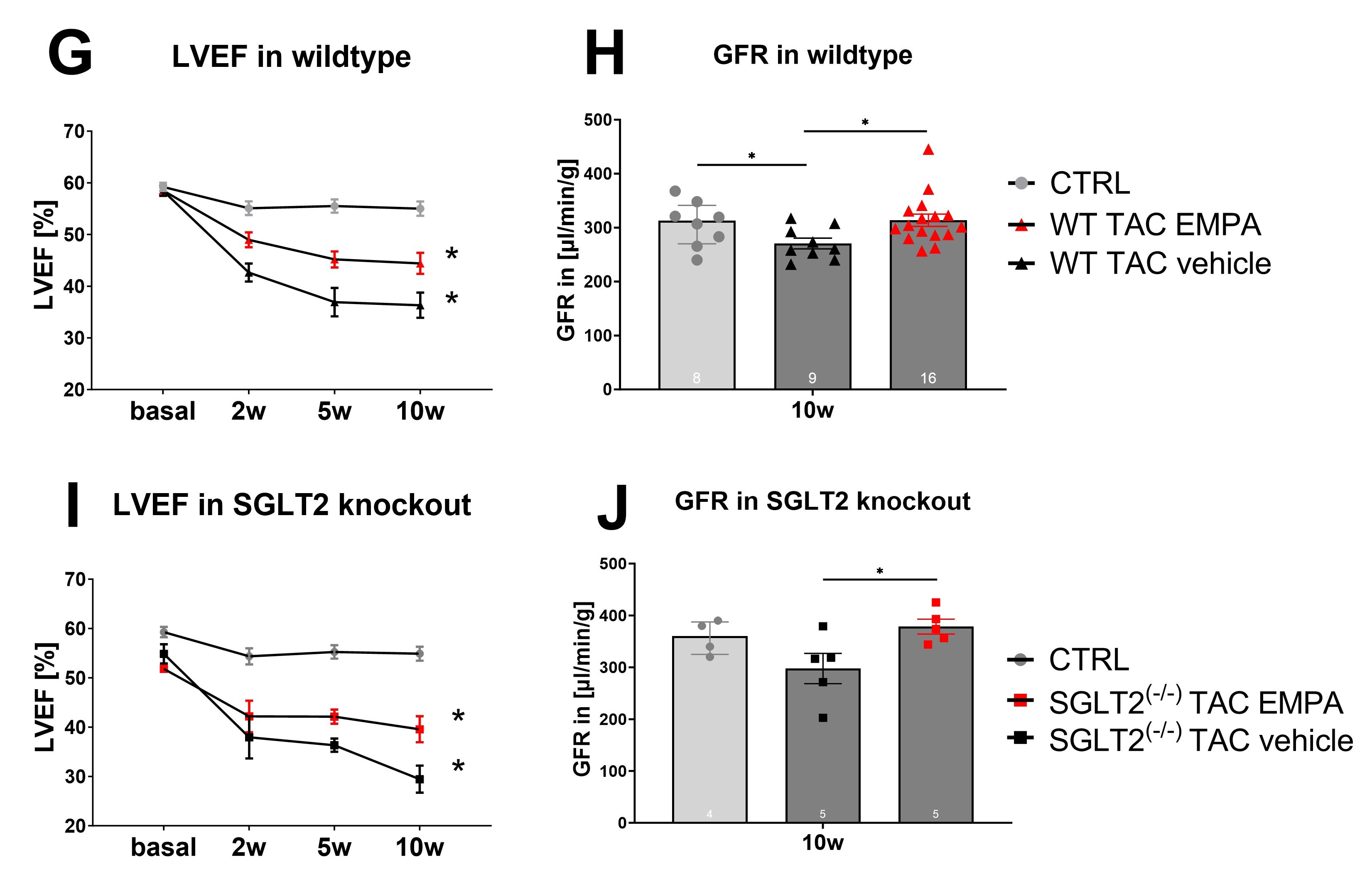
In mice after 10 weeks, echocardiography confirmed TAC induced pressure-overload, leading to reduced LVEF, which was attenuated by EMPA (Fig. G). Interestingly, at 10 weeks, TAC also reduced GFR, which was prevented by EMPA (Fig. H). To test if direct inhibition of SGLT2 is mechanistically involved, TAC surgery was repeated in SGLT2-deficient mice (SGLT2-KO). In fact, exposure to TAC resulted in comparable reduction of LVEF in SGLT2-KO and EMPA prevented this deterioration similar to WT mice (Fig. G vs. I). Surprisingly, EMPA also prevented GFR deterioration 10 weeks after TAC in SGLT2-KO mice with comparable magnitude as in WT mice (Fig. J), suggesting that the reno-protective effect of Empagliflozin was independent from SGLT2 inhibition.
Conclusion and Outlook: This is the first study investigating the role of SGLT2 in Empagliflozin-dependent kidney protection in patients and of mice with heart failure. Importantly, Empagliflozin treatment prevented deterioration of LVEF and GFR independent of the presence of SGLT2.
We hypothesized that Empagliflozin treatment improves left ventricular ejection fraction (LVEF) and thereby renal function in patients and mice independent of renal SGLT2 inhibition.
Methods: We evaluated LVEF and GFR in our patients with HF with reduced (n=32) and preserved ejection fraction (n=59) after 30 and 180 days (prospective, single-arm CINNAMON-study, DRKS00031101). Furthermore, we conducted transverse aortic constriction (TAC) in C57BL/6J (wildtype, WT) and SGLT2 deficient mice (SGLT2-KO). Animals received either Empagliflozin (10 mg/kg bw) or vehicle. Cardiac function was evaluated by echocardiography and kidney function by FITC-Sinistrin measurement (GFR).
Results: Empagliflozin treatment improved LVEF in patients with reduced LVEF whereas in patients with preserved LVEF (Fig. A, B) there was no change in LVEF (Fig. C). Interestingly, only in patients with LVEF < 40% there was a parallel improvement in GFR (Fig. D, E), whereas in patients with LVEF > 40% we only observed the well-known transient drop of GFR (Fig. F).
In mice after 10 weeks, echocardiography confirmed TAC induced pressure-overload, leading to reduced LVEF, which was attenuated by EMPA (Fig. G). Interestingly, at 10 weeks, TAC also reduced GFR, which was prevented by EMPA (Fig. H). To test if direct inhibition of SGLT2 is mechanistically involved, TAC surgery was repeated in SGLT2-deficient mice (SGLT2-KO). In fact, exposure to TAC resulted in comparable reduction of LVEF in SGLT2-KO and EMPA prevented this deterioration similar to WT mice (Fig. G vs. I). Surprisingly, EMPA also prevented GFR deterioration 10 weeks after TAC in SGLT2-KO mice with comparable magnitude as in WT mice (Fig. J), suggesting that the reno-protective effect of Empagliflozin was independent from SGLT2 inhibition.
Conclusion and Outlook: This is the first study investigating the role of SGLT2 in Empagliflozin-dependent kidney protection in patients and of mice with heart failure. Importantly, Empagliflozin treatment prevented deterioration of LVEF and GFR independent of the presence of SGLT2.
More abstracts on this topic:
Foxe1 Loss of Function Contributes to Adverse Remodeling in the Heart
Widiapradja Alexander, Connery Heather, Bullock Martyn, Clifton-bligh Roderick, Levick Scott
Cardiac Catheterization in Kidney Transplant Patients Presenting with Non-ST Segment Elevation Myocardial Infarction: A Five-year Nationwide AnalysisAl Akeel Mohannad, Eldawud Daoud, Jha Mayank, Harikrishna Arya, Jain Hritvik, Abdulfattah Ammar, Alamro Yazan, Patel Jeetendra