Final ID: 4144765
Delayed Management in the Borderline Left Heart Provides Additional Insight Into the Left Heart Potential
Abstract Body (Do not enter title and authors here): Introduction: Prediction of successful biventricular outcome following a fetal diagnosis of borderline left heart (BLH) can be challenging. A postnatal algorithm of delaying interventional decisions to allow for optimized left heart preload and consequent growth was therefore developed. We review our experience, examining changes in left heart dimensions and clinical outcomes using this algorithm.
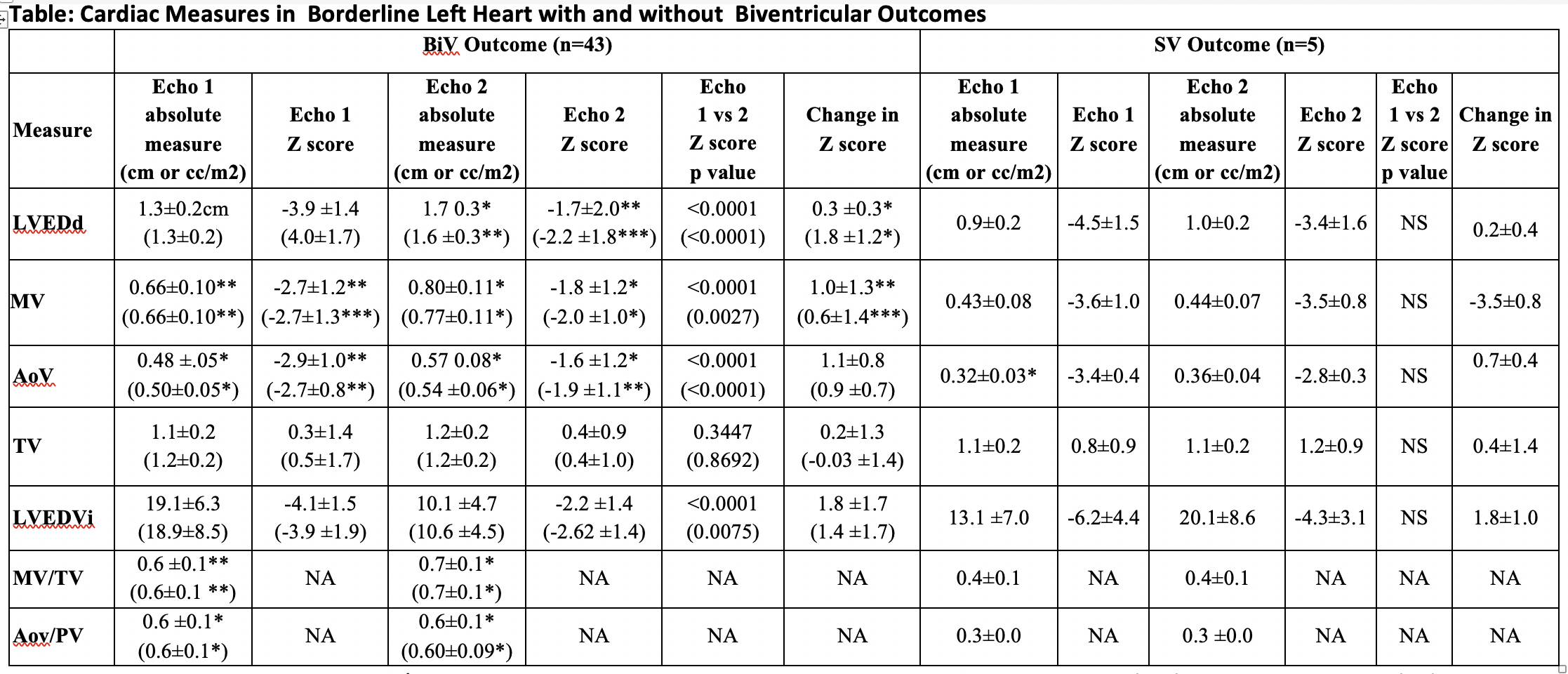
Methods: We identified all fetal BLH cases encountered in our institution from 9/2008-4/2024 with neonatal management and a repeat postnatal preintervention echo available. BLH was defined as a left ventricular (LV) end diastolic dimension(LVEDd) and/or mitral valve(MV) diameter (4 chamber) z score of <-2 at last fetal echo. Pre and postnatal medical records were reviewed. Z-scores of LVEDd, MV and aortic valve(AoV) diameters and LV end diastolic volume indexed to body surface area(LVEDVi)), and left/right heart ratios were compared between initial neonatal echo and either last echo before intervention or at <6 weeks in those without intervention. Findings were also compared between those with vs without a successful biventricular(BiV) outcome.
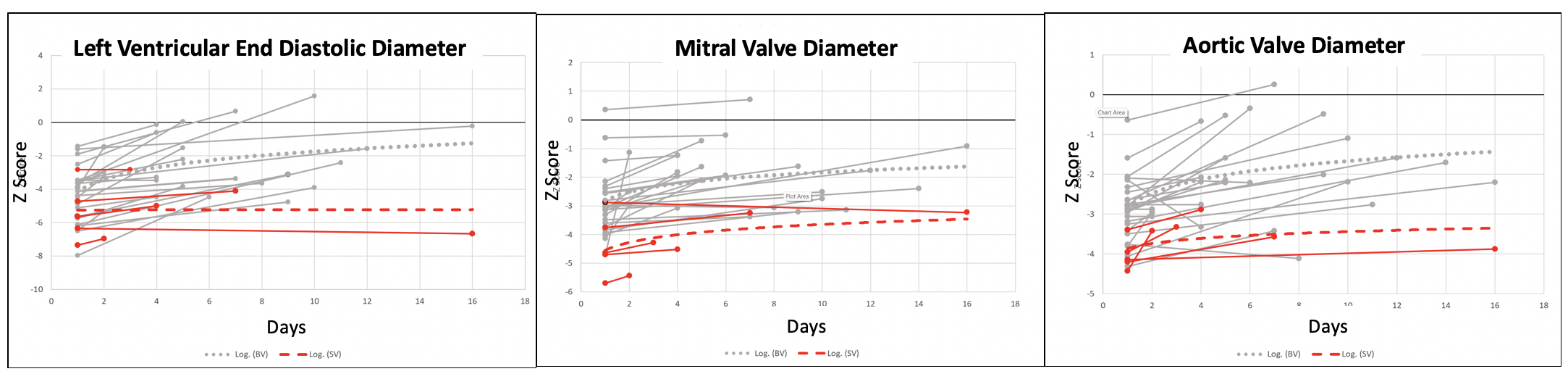
Results: Forty-eight fetuses with a BLH were included. Mean gestational age at last fetal echo was 35.2±2.4 weeks and at birth 38.3±2.0 weeks, and birth weight was 3.0±0.7Kg. Successful BiV outcome occurred in 43(90%), 35 following neonatal intervention (31 with coarctation/arch repair +/- ventricular septal defect), whereas, 5(10%) required single ventricle(SV) palliation (Norwood in 4, transplant with failed BiV repair in 1). Findings at initial (day 1) and repeat echo (BiV 13.8±12.9 and SV 6.4±5.1 days) are presented in the table. Initial MV and AoV diameters and left/right valve ratios were greater and there was a significant increase in size with time for LVEDd, MV and AoV in the BiV compared to the SV group (Table, Figure). When comparing only BiV neonates with surgical intervention who had a similar interval to 2nd study as SV neonates (6.7 ±3.7days), significant increase in LVEDd and MV size occurred in BiV but not SV neonates. All but 1 BiV infant (noncardiac death at 5 months), survived with mean age at last follow-up of 6.0±4.4years.
Conclusions: Delayed decision making confers valuable data about the left heart potential in the BLH newborn. Smaller initial MV and AoV and little or no change in LVED and MV dimensions may be useful in identifying those who should undergo SV palliation.
Methods: We identified all fetal BLH cases encountered in our institution from 9/2008-4/2024 with neonatal management and a repeat postnatal preintervention echo available. BLH was defined as a left ventricular (LV) end diastolic dimension(LVEDd) and/or mitral valve(MV) diameter (4 chamber) z score of <-2 at last fetal echo. Pre and postnatal medical records were reviewed. Z-scores of LVEDd, MV and aortic valve(AoV) diameters and LV end diastolic volume indexed to body surface area(LVEDVi)), and left/right heart ratios were compared between initial neonatal echo and either last echo before intervention or at <6 weeks in those without intervention. Findings were also compared between those with vs without a successful biventricular(BiV) outcome.
Results: Forty-eight fetuses with a BLH were included. Mean gestational age at last fetal echo was 35.2±2.4 weeks and at birth 38.3±2.0 weeks, and birth weight was 3.0±0.7Kg. Successful BiV outcome occurred in 43(90%), 35 following neonatal intervention (31 with coarctation/arch repair +/- ventricular septal defect), whereas, 5(10%) required single ventricle(SV) palliation (Norwood in 4, transplant with failed BiV repair in 1). Findings at initial (day 1) and repeat echo (BiV 13.8±12.9 and SV 6.4±5.1 days) are presented in the table. Initial MV and AoV diameters and left/right valve ratios were greater and there was a significant increase in size with time for LVEDd, MV and AoV in the BiV compared to the SV group (Table, Figure). When comparing only BiV neonates with surgical intervention who had a similar interval to 2nd study as SV neonates (6.7 ±3.7days), significant increase in LVEDd and MV size occurred in BiV but not SV neonates. All but 1 BiV infant (noncardiac death at 5 months), survived with mean age at last follow-up of 6.0±4.4years.
Conclusions: Delayed decision making confers valuable data about the left heart potential in the BLH newborn. Smaller initial MV and AoV and little or no change in LVED and MV dimensions may be useful in identifying those who should undergo SV palliation.
More abstracts on this topic:
A Comparison Between Global Longitudinal Strain (GLS) Derived with CMR Feature-Tracking (CMR-FT) and 2D Speckle-Tracking Echocardiography (2D-STE) to Monitor Cancer Therapy-Related Cardiac Dysfunction (CTRCD)
Kar Julia, Cohen Michael, Revere Cherie, Mcquiston Samuel, Malozzi Christopher
22q11 Deletion Syndrome: A Potenitial Risk Factor For Left Pulmonary Artery Hypoplasia and Need For Intervention in Patients With Congeital Heart DiseaseOliver Shannon, Ward Cameron