Final ID: MDP212
Evaluating Electrocardiographic Predictors of Left Ventricular Ejection Fraction Decline after Conduction System Pacing: Using Time-to-notch in Lead I
Abstract Body (Do not enter title and authors here):
Background: While conduction system pacing (CSP) has shown promise in mitigating the risk of pacemaker-induced cardiomyopathy compared to traditional right ventricular pacing, some patients undergoing CSP may experience declines in left ventricular ejection fraction (LVEF). We aimed to identify ECG predictors of LVEF decline after left bundle branch area pacing (LBBAP) or deep septal pacing (DSP).
Methods: Consecutive patients undergoing LBBAP or DSP at a single center who had baseline LVEF >35%, follow-up echocardiogram at least 90 days post-implant, >20% ventricular pacing, and no coronary intervention during follow-up were retrospectively studied. Post-implant ECGs were analyzed for LBBAP capture (delayed RV activation with RSR’ pattern in V1 or QRS duration <120 msec) or DSP (all others), V6 R wave peak time (<75 msec if narrow QRS or RBBB, <85 msec if LBBB), lead I time to notch >75 msec, and RS/rS pattern in V6. Primary outcome was absolute LVEF decline ≥15%.
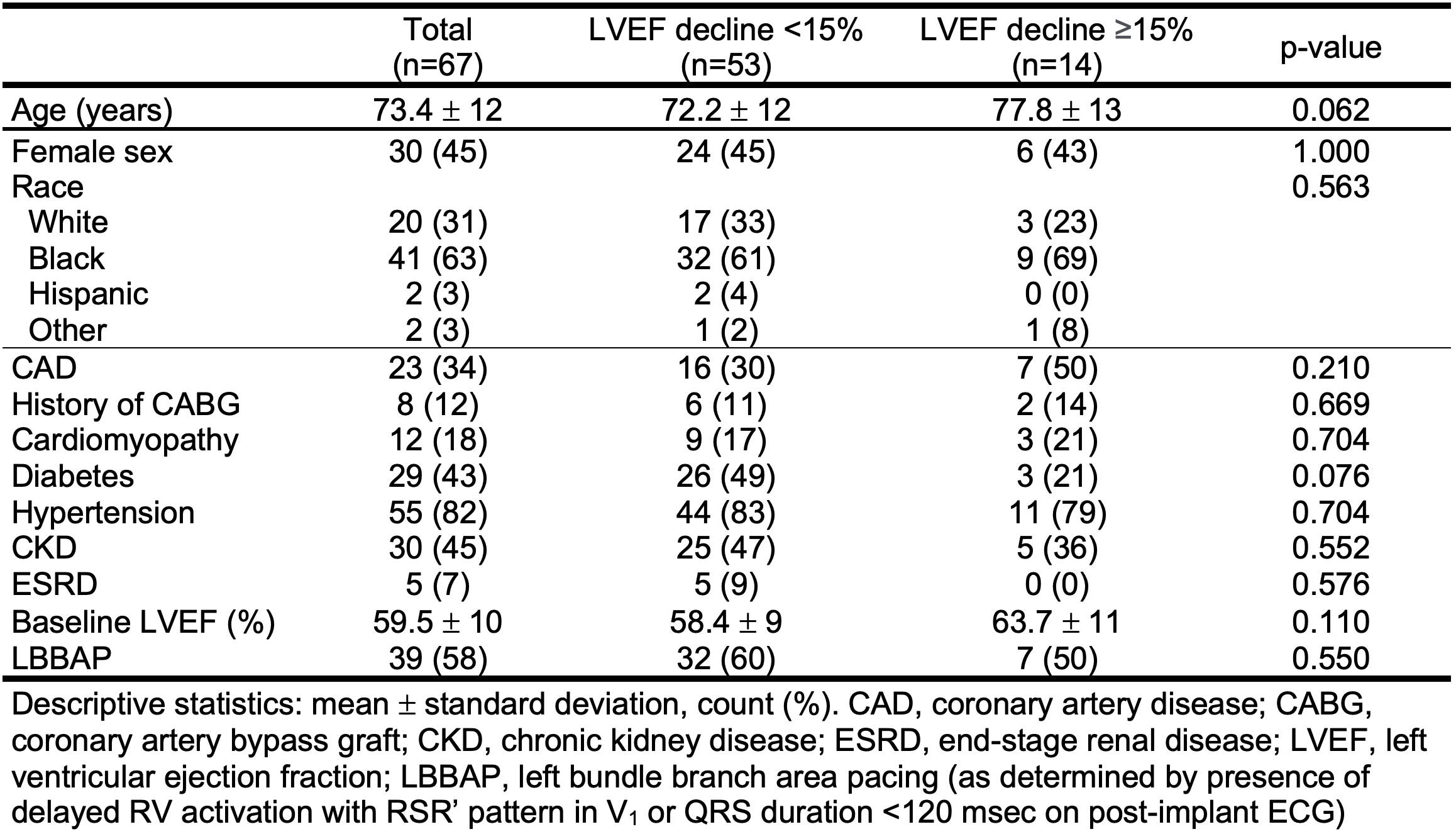
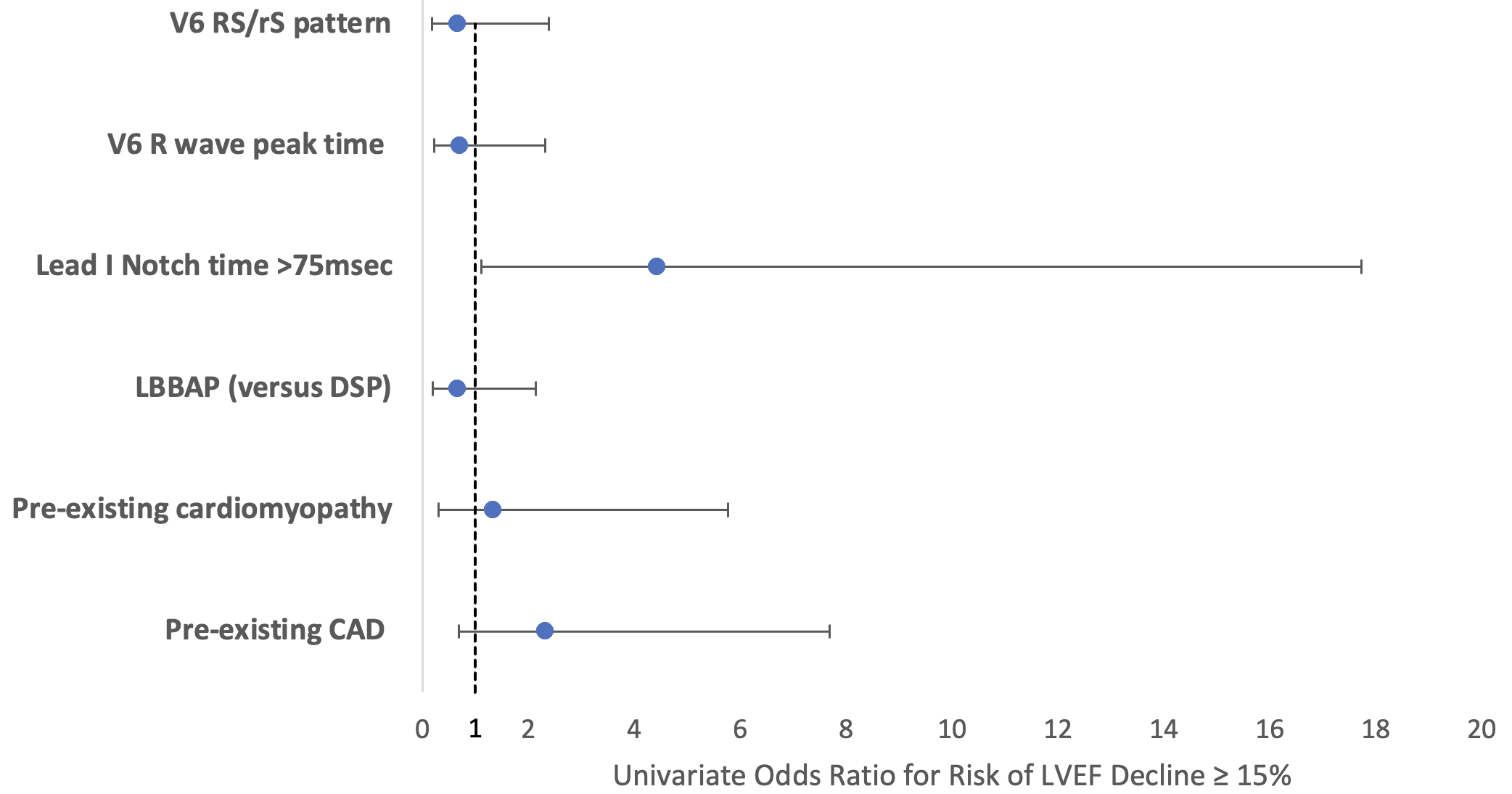
Results: A total of 67 patients met inclusion criteria with mean age 73 years, 45% female, 63% African American, 34% CAD, 18% cardiomyopathy, and 60% median LVEF (IQR 52-68%) at baseline. LBBAP was achieved in 39 (58%) and DSP in 28 (42%). Median pacing at follow-up was 99% over median follow-up of 15.6 (IQR 8-23) months. No differences were noted with respect to demographics, clinical comorbidities, or LBBAP vs DSP among patients with and without LVEF decline ≥15% (Table). Among ECG predictors, notch time in Lead I >75 msec was significant on univariate logistic regression analysis (OR 4.431, 95% CI 1.11-17.72, p=0.035, Figure) and with multivariate adjustment for age, baseline LVEF, history of cardiomyopathy or CAD.
Conclusion: Lead I notch time >75 msec on post-implant paced ECG was associated with LVEF decline at follow up, albeit with broad confidence intervals. These findings suggest utility in evaluating paced QRS patterns after CSP to identify patients at risk for pacemaker-induced cardiomyopathy.
Background: While conduction system pacing (CSP) has shown promise in mitigating the risk of pacemaker-induced cardiomyopathy compared to traditional right ventricular pacing, some patients undergoing CSP may experience declines in left ventricular ejection fraction (LVEF). We aimed to identify ECG predictors of LVEF decline after left bundle branch area pacing (LBBAP) or deep septal pacing (DSP).
Methods: Consecutive patients undergoing LBBAP or DSP at a single center who had baseline LVEF >35%, follow-up echocardiogram at least 90 days post-implant, >20% ventricular pacing, and no coronary intervention during follow-up were retrospectively studied. Post-implant ECGs were analyzed for LBBAP capture (delayed RV activation with RSR’ pattern in V1 or QRS duration <120 msec) or DSP (all others), V6 R wave peak time (<75 msec if narrow QRS or RBBB, <85 msec if LBBB), lead I time to notch >75 msec, and RS/rS pattern in V6. Primary outcome was absolute LVEF decline ≥15%.
Results: A total of 67 patients met inclusion criteria with mean age 73 years, 45% female, 63% African American, 34% CAD, 18% cardiomyopathy, and 60% median LVEF (IQR 52-68%) at baseline. LBBAP was achieved in 39 (58%) and DSP in 28 (42%). Median pacing at follow-up was 99% over median follow-up of 15.6 (IQR 8-23) months. No differences were noted with respect to demographics, clinical comorbidities, or LBBAP vs DSP among patients with and without LVEF decline ≥15% (Table). Among ECG predictors, notch time in Lead I >75 msec was significant on univariate logistic regression analysis (OR 4.431, 95% CI 1.11-17.72, p=0.035, Figure) and with multivariate adjustment for age, baseline LVEF, history of cardiomyopathy or CAD.
Conclusion: Lead I notch time >75 msec on post-implant paced ECG was associated with LVEF decline at follow up, albeit with broad confidence intervals. These findings suggest utility in evaluating paced QRS patterns after CSP to identify patients at risk for pacemaker-induced cardiomyopathy.
More abstracts on this topic:
A Risk Prediction Score for Shockable Sudden Cardiac Arrest: Validation in the Framingham Heart Study
Truyen Thien Tan Tri Tai, Lin Honghuang, Mathias Marco, Chugh Harpriya, Reinier Kyndaron, Benjamin Emelia, Chugh Sumeet
Anatomic Physiological Scoring is a Comparable Predictor of Adult Congenital Operative Morbidity and MortalityLa Brenda, Taylor-fishwick Jon, Macbeth Morgan, Soohoo Megan