Final ID: Su2015
Socioeconomic and Geographic Factors Associated with Reduced Prenatal Diagnosis of Significant Congenital Heart Disease at a Single Regional Institution
Abstract Body (Do not enter title and authors here): Background: Prenatal diagnosis (PND) of congenital heart disease (CHD) is associated with lower preoperative mortality and improved perinatal outcomes. Socioeconomic (SE) and geographic disparities impact PND of CHD in the United States. However, the relationship of these disparities and PND along with postnatal outcomes have not been previously studied in the Northwestern United States, a large geographic catchment area with significant SE and access-to-care variability.
Hypothesis: Greater SE disadvantage, defined by higher Area Deprivation Index (ADI), as well as non-white race, Hispanic ethnicity and increased distance from our regional surgical center are associated with lower rates of PND of CHD.
Aims: To evaluate the association of SE and geographic variables and PND of CHD in a cardiac center with a unique catchment area. Also to compared post-operative outcomes between those diagnosed prenatally and postnatally.
Methods: A Retrospective cross-sectional study of all patients with CHD requiring surgical intervention <6 months of age between 2014-202 at a single institution, serving 6 states, in the Northwestern United States was performed. Medical records, prenatal, and surgical databases provided demographic, diagnosis, and outcomes data. Race, ethnicity, ADI and address data were collected from first hospitalization or prenatal record depending on timing of diagnosis.
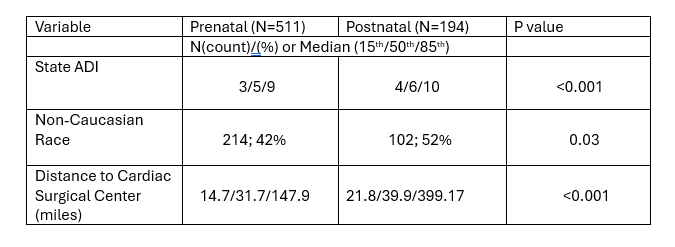
Results: 705 patients met inclusion criteria; 511 prenatally diagnosed and 194 postnatally. Higher (more disadvantaged) State ADI (p<0.001), non-white race (p=0.03), Hispanic ethnicity (p<0.002) and increased distance from surgical center (p<0.001) were associated with lower rates of prenatal diagnosis. No significant difference in post-surgical variables between prenatally and postnatally diagnosed patients was found.
Conclusion: In a large regional catchment area serviced by a single surgical center, non-white race, Hispanic ethnicity, higher state ADI and distance from regional surgical center were associated with decreased rates of PND of significant CHD. This study provides a framework for developing strategies to improve accessibility to comprehensive prenatal care for underserved communities.
Hypothesis: Greater SE disadvantage, defined by higher Area Deprivation Index (ADI), as well as non-white race, Hispanic ethnicity and increased distance from our regional surgical center are associated with lower rates of PND of CHD.
Aims: To evaluate the association of SE and geographic variables and PND of CHD in a cardiac center with a unique catchment area. Also to compared post-operative outcomes between those diagnosed prenatally and postnatally.
Methods: A Retrospective cross-sectional study of all patients with CHD requiring surgical intervention <6 months of age between 2014-202 at a single institution, serving 6 states, in the Northwestern United States was performed. Medical records, prenatal, and surgical databases provided demographic, diagnosis, and outcomes data. Race, ethnicity, ADI and address data were collected from first hospitalization or prenatal record depending on timing of diagnosis.
Results: 705 patients met inclusion criteria; 511 prenatally diagnosed and 194 postnatally. Higher (more disadvantaged) State ADI (p<0.001), non-white race (p=0.03), Hispanic ethnicity (p<0.002) and increased distance from surgical center (p<0.001) were associated with lower rates of prenatal diagnosis. No significant difference in post-surgical variables between prenatally and postnatally diagnosed patients was found.
Conclusion: In a large regional catchment area serviced by a single surgical center, non-white race, Hispanic ethnicity, higher state ADI and distance from regional surgical center were associated with decreased rates of PND of significant CHD. This study provides a framework for developing strategies to improve accessibility to comprehensive prenatal care for underserved communities.
More abstracts on this topic:
Age and Sex Multiplicatively Moderate the Association of Daily Sedentary Time with Depressive Symptoms in Rural Patients with Cardiovascular Diseases
Kang Junghee, Moser Debra, Cha Geunyeong, Lin Chin-yen, Wu Jia-rong, Okoli Chizimuzo, Latimer Abigail, Lennie Terry, Biddle Martha, Chung Misook
Adherence to Pediatric Screening Guidelines for Cardiovascular Risk Factors in a Diverse Cohort of Children in ChicagoGauen Abigail, Wang Yaojie, Perak Amanda, Davis Matthew, Rosenman Marc, Lloyd-jones Donald, Zmora Rachel, Allen Norrina, Petito Lucia