Final ID: Sa3055
Attenuation of Black-White Disparities in Cardiovascular Disease Incidence and Total Mortality by Life’s Essential 8: Cardiovascular Lifetime Risk Pooling Project (LRPP)
Abstract Body (Do not enter title and authors here): Background: Higher cardiovascular health (CVH), as measured by Life’s Essential 8 (LE8) score, is associated with lower mortality and incident cardiovascular disease (CVD). It is unclear if having higher CVH attenuates racial disparities in CVD and total mortality.
Methods: We used data from the LRPP, including the ARIC, CARDIA, MESA, and Framingham Offspring cohorts, for which LE8 scores (0-100 points, higher is better) could be calculated in participants (ppts) aged 20-59 years who self-identified as Black or White. We compared incidence rates and adjusted hazard ratios (aHR; adjusted for age, sex, and maximal education years) for incident CVD and total mortality between Black and White ppts. We estimated the quantitative reduction in Black-White hazards without vs. with adjustment for LE8 score by examining the proportional change in the beta coefficients.
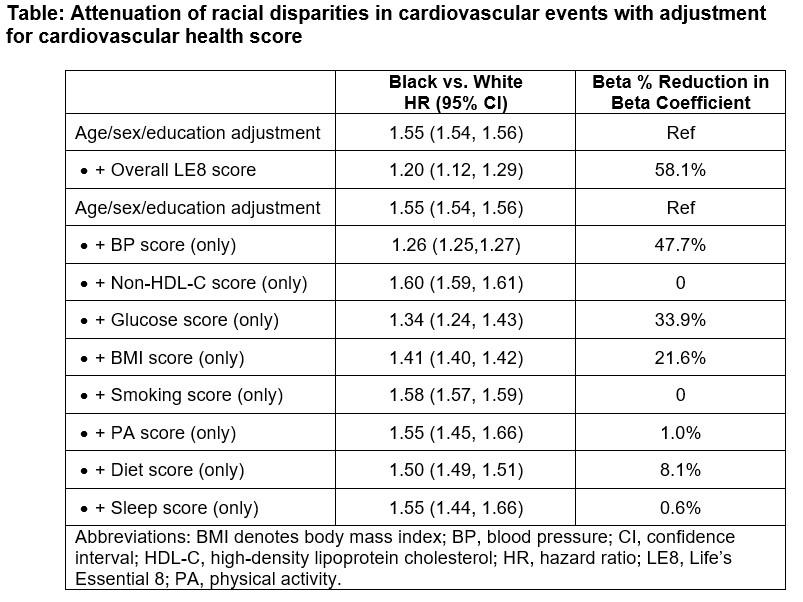
Results: Our sample included 20,618 ppts (28.6% Black; 54.8% women; mean age 45.9±11.6 years) followed for 499 000 person-years, of whom 4316 developed CVD events and 5660 died. Mean LE8 score was 66.4±14.3 for White and 61.5±14.7 for Black ppts. Among White ppts, 19.9% had a CVD event and 25.8% died, compared to 23.4% and 31.7% of Black ppts, respectively. Compared with White ppts, Black adults had higher hazards for incident CVD (aHR 1.55; 95% CI 1.54-1.56). Additional adjustment for LE8 score attenuated the HR to 1.20 (95% CI 1.12-1.29), representing a 58.1% reduction in the beta estimate for race (see Table). Considering LE8 metrics individually, adjustment for blood pressure score was associated with the greatest proportional reduction in the Black-White beta estimate (47.7%). Findings were overall similar for associations and attenuation of racial disparities in total mortality, with a 39.9% reduction in the beta estimate for Black vs. White ppts.
Conclusions: In young and middle-aged adults, adjustment for cardiovascular health score partially attenuated Black-White disparities in incident CVD events and mortality. It is likely that the observed disparities are based on social and structural determinants. Improving CVH from young adulthood could be an important strategy for reducing racial disparities in CVD events and mortality.
Methods: We used data from the LRPP, including the ARIC, CARDIA, MESA, and Framingham Offspring cohorts, for which LE8 scores (0-100 points, higher is better) could be calculated in participants (ppts) aged 20-59 years who self-identified as Black or White. We compared incidence rates and adjusted hazard ratios (aHR; adjusted for age, sex, and maximal education years) for incident CVD and total mortality between Black and White ppts. We estimated the quantitative reduction in Black-White hazards without vs. with adjustment for LE8 score by examining the proportional change in the beta coefficients.
Results: Our sample included 20,618 ppts (28.6% Black; 54.8% women; mean age 45.9±11.6 years) followed for 499 000 person-years, of whom 4316 developed CVD events and 5660 died. Mean LE8 score was 66.4±14.3 for White and 61.5±14.7 for Black ppts. Among White ppts, 19.9% had a CVD event and 25.8% died, compared to 23.4% and 31.7% of Black ppts, respectively. Compared with White ppts, Black adults had higher hazards for incident CVD (aHR 1.55; 95% CI 1.54-1.56). Additional adjustment for LE8 score attenuated the HR to 1.20 (95% CI 1.12-1.29), representing a 58.1% reduction in the beta estimate for race (see Table). Considering LE8 metrics individually, adjustment for blood pressure score was associated with the greatest proportional reduction in the Black-White beta estimate (47.7%). Findings were overall similar for associations and attenuation of racial disparities in total mortality, with a 39.9% reduction in the beta estimate for Black vs. White ppts.
Conclusions: In young and middle-aged adults, adjustment for cardiovascular health score partially attenuated Black-White disparities in incident CVD events and mortality. It is likely that the observed disparities are based on social and structural determinants. Improving CVH from young adulthood could be an important strategy for reducing racial disparities in CVD events and mortality.
More abstracts on this topic:
A Blood(y) Pressure Crisis: Diffuse Alveolar Hemorrhage as a Rare Manifestation of Severely Uncontrolled Hypertension
Nandyal Shreyas, Amdetsion Gedion Yilma, Varma Revati, Kohli Saksham, Hammo Hasan
A Multi-Center Clinic Site Comparison of Patient-level factors Affecting Oral Anticoagulation Prescription for Atrial FibrillationIqbal Fatima, Hoang Kenneth, Chiadika Simbo