Final ID: Mo2036
Single Center Rates and Trends in Diagnosis of Necrotizing Enterocolitis in Pediatric Shunt-Dependent Congenital Heart Disease
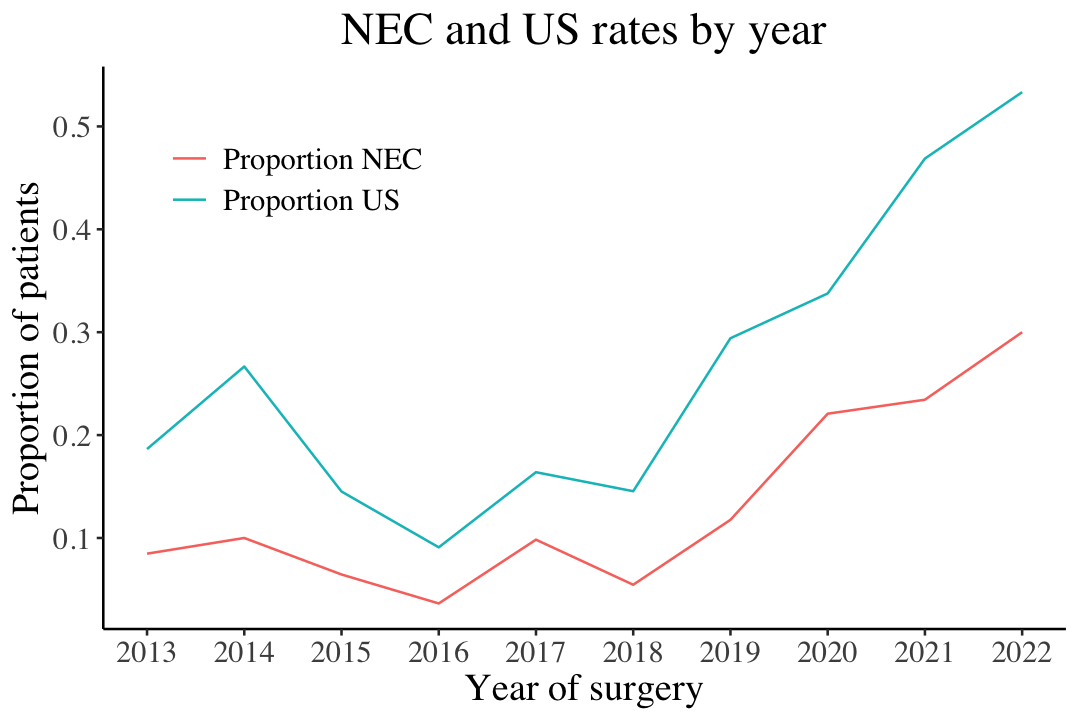
Abstract Body (Do not enter title and authors here): Background: Necrotizing enterocolitis (NEC) is a rare comorbidity in infants with heart disease, specifically those with shunt-dependent congenital heart disease (SDCHD). We aimed to describe NEC incidence and cofactors in our center’s SDCHD population and diagnostic practice changes. Methods: A retrospective case-control study in patients who underwent first staged palliation for SDCHD between 1/1/2013 and 6/30/2022. Palliation procedures included stage one Norwood with a BTTS or RV to PA conduit, hybrid, BTTS only or PDA stent. Demographics, clinical factors, and diagnostics including abdominal ultrasound (AUS) were abstracted for subjects for 21 days after palliation. NEC was defined with Bell’s criteria from databases and AUS was assessed by chart review. Hierarchical logistic regression models assessed surgical era rates into three cohorts 2013-2016, 2017-2019, and 2020-2022. Groups were compared with Chi-square, Fisher’s exact test, Wilcoxon rank-sum tests, and trends over time with logistical regression. Results: Of 531 patients included, 77 (14.5%) had NEC. There was no association of NEC diagnosis with sex, race, and ethnicity, presence of genetic syndromes or extracardiac abnormalities. The primary and majority SDCHD diagnosis was hypoplastic left heart syndrome and variants (61%). On univariate analysis, risks significantly associated with NEC include younger gestational age, delayed sternal closure, catheter reintervention, ECMO, cardiac arrest, seizures, >/= moderate ventricular dysfunction, increased pre- and post-procedural VIS scores, and postoperative anemia. Logistic regression found a significant increase in NEC by year, with a 23% increase in odds for each increasing year across the time range (OR 1.23, 95% CI 1.12-1.36, p<0.001) and odds of AUS use significantly increased by year (OR 1.14, 95% CI 1.05-1.24, p=0.003). When controlling for gestational age, procedure type, presence of a genetic syndrome and chromosomal abnormality the odds of having a NEC diagnosis increased by 1.24 on average with each change in era. Conclusions: Rates of NEC diagnoses at our institution have increased over time with ultrasound as a diagnostic indicator. Clinical risks factors suggesting higher acuity of illness were associated with higher rates of NEC. Further studies are needed to assess AUS sensitivity and its contribution to NEC rates, as well as a multicenter analysis to collate risk factors for this fragile patient population.
More abstracts on this topic:
Angiography-based pulmonary capillary transit time is a promising diagnostic tool for single ventricle pulmonary arteriovenous malformations
Bergstrand David, Spearman Andrew
An Electronic Health Record Multimodal Data Integration Platform for Comprehensive Analysis of Single Ventricle PhysiologyXu Hang, Aboulhosn Jamil, Christodoulou Anthony, Finn Paul, Hsu William, Nguyen Kimlien, Zhang Hinn, Sisniega Carlos, Renella Pierangelo, Morris Connor, Husain Majid, Satou Gary, Zhu Bing, Van Arsdell Glen