Final ID: Sa3057
Racial Disparities in Age-adjusted Sudden Cardiac Death Rates in the United States: Insights from CDC-WONDER Database, 1999-2020
Abstract Body (Do not enter title and authors here): Hypothesis: Small prospective and dataset-based studies predicted the rates of sudden cardiac death (SCD) are higher in the African American (AA) population as compared to White Americans (WA). However, there is a lack of long-term data over two decades looking
for racial differences in SCD.
Aim: Our study aims to analyze and quantify the racial differences in age-adjusted mortality rates(AAMR) related to SCDs between AA and WA to further explore potential contributing factors, such as socioeconomic status, sex, and varied comorbidity burdens, to these differences.
Methods: We analyzed the Centers for Disease Control and Prevention (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER) database, containing death certificate records for various causes of mortality in the US from 1999 to 2020. We searched the CDC WONDER database for patients, 18-45 years old whose cause of death was SCD corresponding to ICD-10 code; I46.1. We searched for AAMR and stratified patients based on race and gender on a total population of 48668 (41975 WA; 6693 AA). Temporal trends were analyzed by fitting log-linear regression models using the Joinpoint Regression Program.
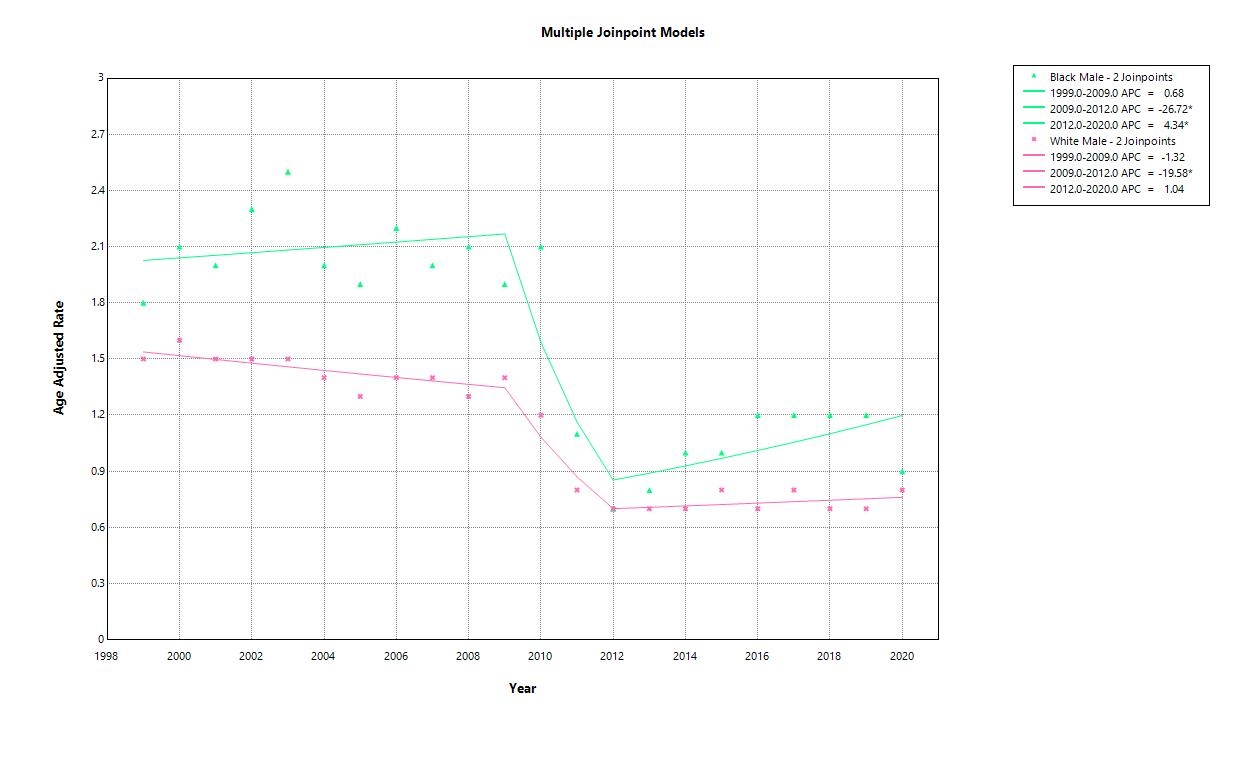
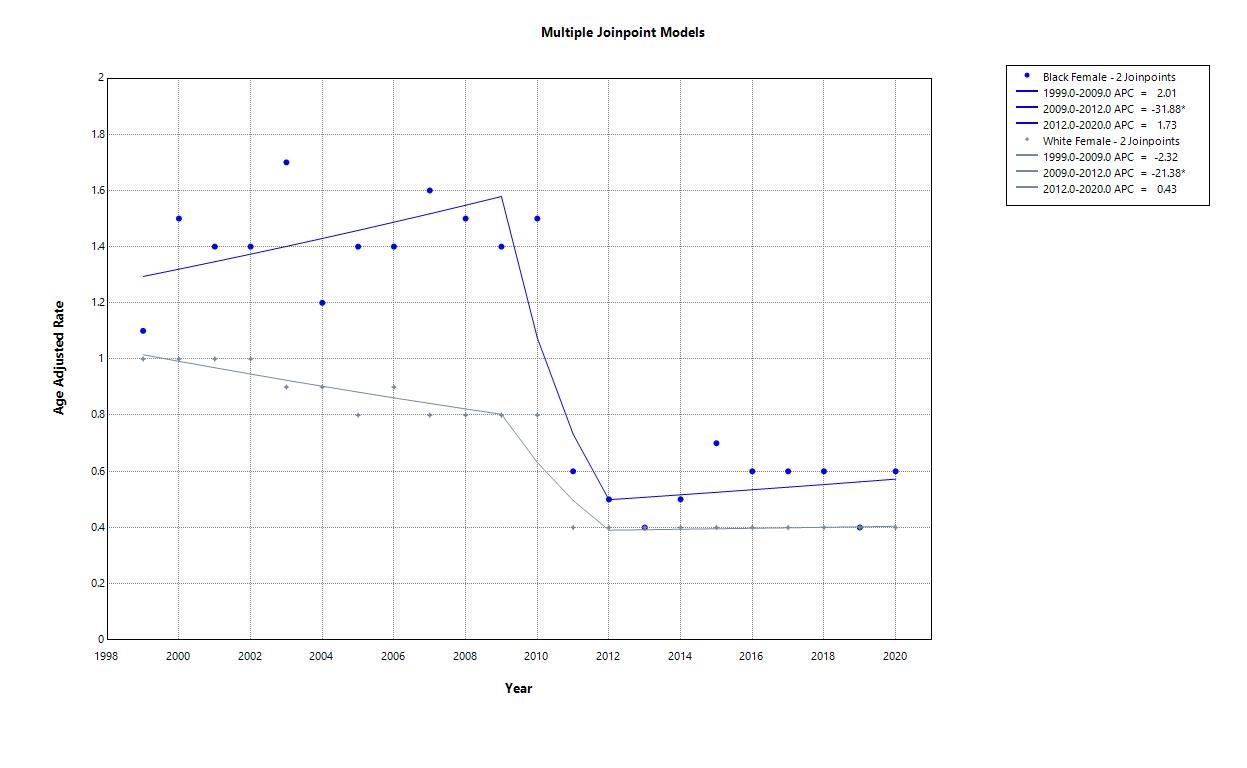
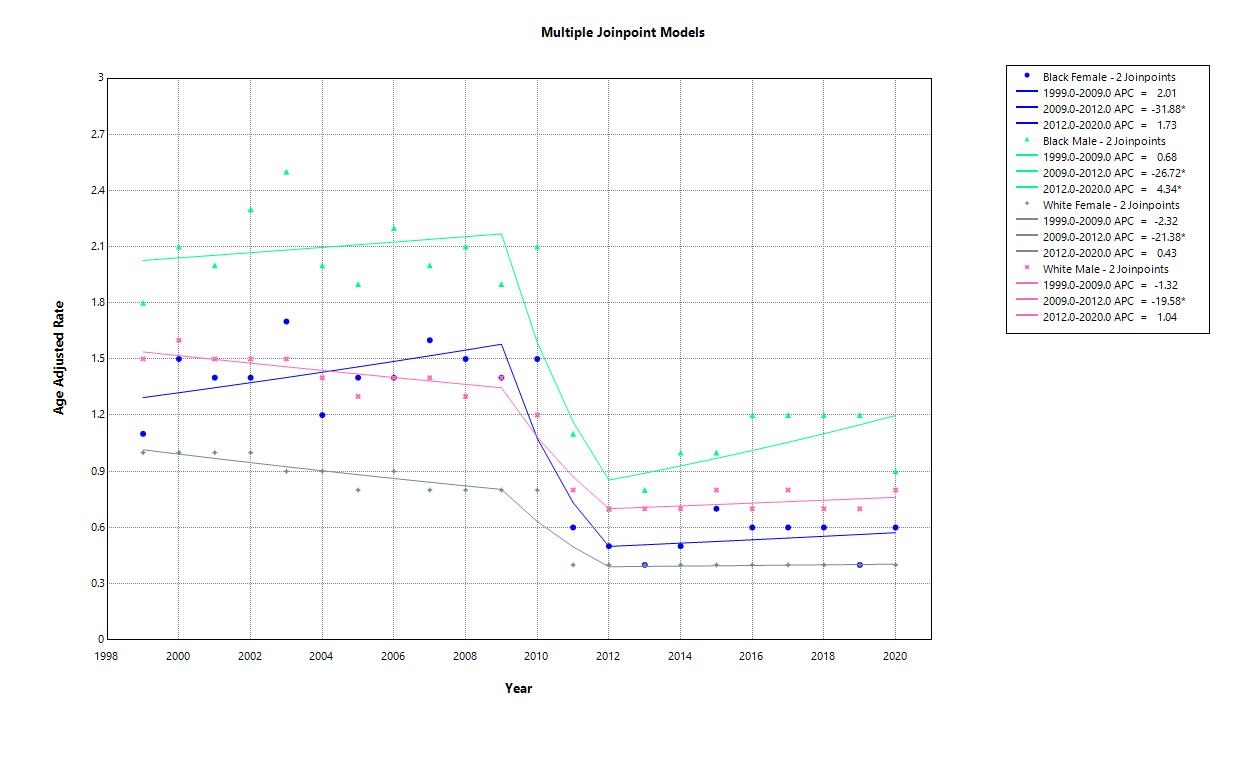
Results: We calculated annual percent change (APC) with 95% confidence intervals (CIs) in AAMR for the line segments linking joint points. The AAMR for SCDs in AA males ranged from 2.1% in 2000 to 0.9% in 2020 with an APC of 0.68 between 1999 and 2009, -26.72 between 2009 and 2012, and 4.34 between 2012 and 2020 suggest that the rate peaked between 2008 and 2010, followed by a significant decline in the following years. WA males had consistently lower rates compared to AA males. The AAMR for WA males peaked at 1.5% in 2000 followed by a stepwise decline until it reached a rate less than 0.9% in 2020, with APCs -1.32 between 1999 and 2009, -19.58 between 2009 and 2012. [Figure A]. AA females had APCs of 2.01, -31.88, and 1.73 while WA females had APCs of -2.32, -21.38, and 0.43 between 1999 and 2009, 2009 and 2012, and 2012 and 2020, respectively [Figure B]. Rates in AA females had a similar progression to that in AA males [Figure C].
Conclusion: Racial disparities in SCDs related AAMR in the US suggest the role of a complex interplay between healthcare delivery, underlying pathological processes, and race. AA demonstrated higher age-adjusted SCD rates than WA. These findings should be used to guide policymaking and address areas of unmet need in providing racially equitable healthcare for all patients.
for racial differences in SCD.
Aim: Our study aims to analyze and quantify the racial differences in age-adjusted mortality rates(AAMR) related to SCDs between AA and WA to further explore potential contributing factors, such as socioeconomic status, sex, and varied comorbidity burdens, to these differences.
Methods: We analyzed the Centers for Disease Control and Prevention (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER) database, containing death certificate records for various causes of mortality in the US from 1999 to 2020. We searched the CDC WONDER database for patients, 18-45 years old whose cause of death was SCD corresponding to ICD-10 code; I46.1. We searched for AAMR and stratified patients based on race and gender on a total population of 48668 (41975 WA; 6693 AA). Temporal trends were analyzed by fitting log-linear regression models using the Joinpoint Regression Program.
Results: We calculated annual percent change (APC) with 95% confidence intervals (CIs) in AAMR for the line segments linking joint points. The AAMR for SCDs in AA males ranged from 2.1% in 2000 to 0.9% in 2020 with an APC of 0.68 between 1999 and 2009, -26.72 between 2009 and 2012, and 4.34 between 2012 and 2020 suggest that the rate peaked between 2008 and 2010, followed by a significant decline in the following years. WA males had consistently lower rates compared to AA males. The AAMR for WA males peaked at 1.5% in 2000 followed by a stepwise decline until it reached a rate less than 0.9% in 2020, with APCs -1.32 between 1999 and 2009, -19.58 between 2009 and 2012. [Figure A]. AA females had APCs of 2.01, -31.88, and 1.73 while WA females had APCs of -2.32, -21.38, and 0.43 between 1999 and 2009, 2009 and 2012, and 2012 and 2020, respectively [Figure B]. Rates in AA females had a similar progression to that in AA males [Figure C].
Conclusion: Racial disparities in SCDs related AAMR in the US suggest the role of a complex interplay between healthcare delivery, underlying pathological processes, and race. AA demonstrated higher age-adjusted SCD rates than WA. These findings should be used to guide policymaking and address areas of unmet need in providing racially equitable healthcare for all patients.
More abstracts on this topic:
Adverse Social Determinants of Health in a Low-Income Population Hospitalized with Heart Failure
Rizvi Syed Kazim, Lokesh Nidhish, Dhruve Ritika, Miller James, Keshvani Neil, Pandey Ambarish
A Machine Learning-Derived Socio-Environmental Risk Score More Accurately Predicts Cardiovascular Events and Better Addresses Health Inequities than Social Deprivation IndexChen Zhuo, Nasir Khurram, Al-kindi Sadeer, Rajagopalan Sanjay, Ponnana Sai Rahul, Dazard Jean-eudes, Zhang Tong, Dong Weichuan, Okyere Robert, Sirasapalli Santosh, Deo Salil, Khraishah Haitham